Substance abuse is a complex issue that has significant impacts on individuals, families, and communities. It refers to the harmful or excessive use of drugs, alcohol, or other substances that can lead to a range of physical, psychological, and social problems. While the causes of substance abuse can vary from person to person, the effects are often devastating and can include addiction, health problems, strained relationships, and financial struggles. In this essay, we will explore the common causes and effects of substance abuse and discuss potential strategies for prevention and treatment. By understanding the underlying factors and consequences of substance abuse, we can work towards creating a healthier and safer society for all.
Substance abuse, also known as drug abuse, refers to a maladaptive pattern of use of a substance that is not considered dependent. The term “drug abuse” does not exclude dependency, but is otherwise used in a similar manner in nonmedical contexts. The terms have a huge range of definitions related to taking a psychoactive drug or performance enhancing drug for a non-therapeutic or non-medical effect. All of these definitions imply a negative judgment of the drug use in question (compare with the term responsible drug use for alternative views). Some of the drugs most often associated with this term include alcohol, amphetamines, barbiturates, benzodiazepines (particularly temazepam, nimetazepam, and flunitrazepam), cocaine, methaqualone, and opioids. Use of these drugs may lead to criminal penalty in addition to possible physical, social, and psychological harm, both strongly depending on local jurisdiction. Other definitions of drug abuse fall into four main categories: public health definitions, mass communication and vernacular usage, medical definitions, and political and criminal justice definitions.
Substance abuse is a form of substance-related disorder.
Classification
Public health definitions
Public health practitioners have attempted to look at drug abuse from a broader perspective than the individual, emphasizing the role of society, culture and availability. Rather than accepting the loaded terms alcohol or drug “abuse,” many public health professionals have adopted phrases such as “substance and alcohol type problems” or “harmful/problematic use” of drugs.
The Health Officers Council of British Columbia — in their 2005 policy discussion paper, A Public Health Approach to Drug Control in Canada — has adopted a public health model of psychoactive substance use that challenges the simplistic black-and-white construction of the binary (or complementary) antonyms “use” vs. “abuse”. This model explicitly recognizes a spectrum of use, ranging from beneficial use to chronic dependence (see diagram to the right).
Medical definitions
In the modern medical profession, the two most used diagnostic tools in the world, the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM) and the World Health Organization’s International Statistical Classification of Diseases and Related Health Problems (ICD), no longer recognize ‘drug abuse’ as a current medical diagnosis. Instead, DSM has adopted substance abuse as a blanket term to include drug abuse and other things. ICD refrains from using either “substance abuse” or “drug abuse”, instead using the term “harmful use” to cover physical or psychological harm to the user from use. Physical dependence, abuse of, and withdrawal from drugs and other miscellaneous substances is outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) ). Its section Substance dependence begins with:
“Substance dependence When an individual persists in use of alcohol or other drugs despite problems related to use of the substance, substance dependence may be diagnosed. Compulsive and repetitive use may result in tolerance to the effect of the drug and withdrawal symptoms when use is reduced or stopped. These, along with Substance Abuse are considered Substance Use Disorders….”
However, other definitions differ; they may entail psychological or physical dependence, and may focus on treatment and prevention in terms of the social consequences of substance uses.
Drug misuse
Drug misuse is a term used commonly for prescription medications with clinical efficacy but abuse potential and known adverse effects linked to improper use, such as psychiatric medications with sedative, anxiolytic, analgesic, or stimulant properties. Prescription misuse has been variably and inconsistently defined based on drug prescription status, the uses that occur without a prescription, intentional use to achieve intoxicating effects, route of administration, co-ingestion with alcohol, and the presence or absence of abuse or dependence symptoms. Tolerance relates to the pharmacological property of substances in which chronic use leads to a change in the central nervous system, meaning that more of the substance is needed in order to produce desired effects. Stopping or reducing the use of this substance would cause withdrawal symptoms to occur.
As a value judgment
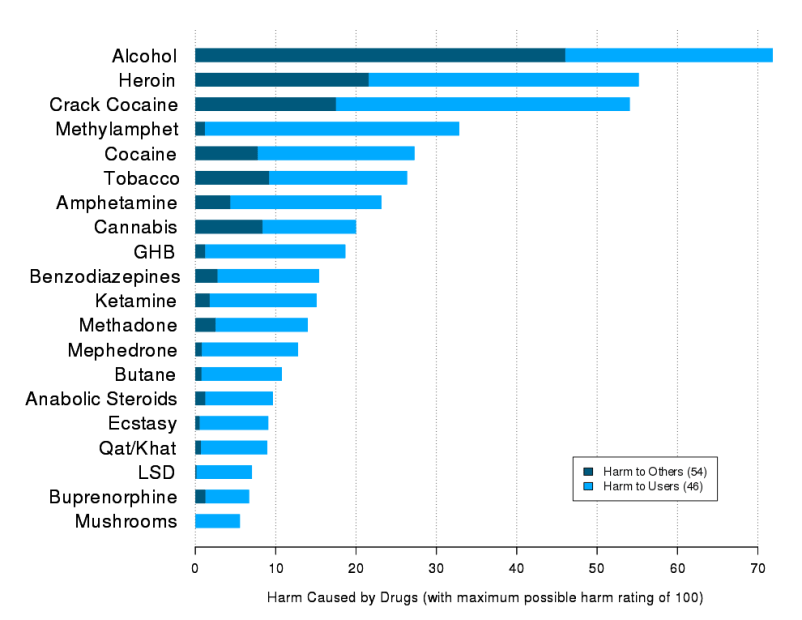 Legal drugs are not necessarily safer. A study in 2010 asked drug-harm experts to rank various illegal and legal drugs. Alcohol was found to be the most dangerous by far.
Legal drugs are not necessarily safer. A study in 2010 asked drug-harm experts to rank various illegal and legal drugs. Alcohol was found to be the most dangerous by far.
Philip Jenkins points out that there are two issues with the term “drug abuse”. First, what constitutes a “drug” is debatable. For instance, GHB, a naturally occurring substance in the central nervous system is considered a drug, and is illegal in many countries, while nicotine is not officially considered a drug in most countries. Second, the word “abuse” implies a recognized standard of use for any substance. Drinking an occasional glass of wine is considered acceptable in many Western countries, while drinking several bottles is seen as an abuse. Strict temperance advocates, which may or may not be religiously motivated, would see drinking even one glass as an abuse, and some groups even condemn caffeine use in any quantity. Similarly, adopting the view that any (recreational) use of marijuana or amphetamines constitutes drug abuse implies that we have already decided that substance is harmful even in minute quantities.
Signs and symptoms
Depending on the actual compound, drug abuse including alcohol may lead to health problems, social problems, morbidity, injuries, unprotected sex, violence, deaths, motor vehicle accidents, homicides, suicides, physical dependence or psychological addiction.
There is a high rate of suicide in alcoholics and other drug abusers. The reasons believed to cause the increased risk of suicide include the long-term abuse of alcohol and other drugs causing physiological distortion of brain chemistry as well as the social isolation. Another factor is the acute intoxicating effects of the drugs may make suicide more likely to occur. Suicide is also very common in adolescent alcohol abusers, with 1 in 4 suicides in adolescents being related to alcohol abuse. In the USA approximately 30 percent of suicides are related to alcohol abuse. Alcohol abuse is also associated with increased risks of committing criminal offences including child abuse, domestic violence, rapes, burglaries and assaults.
Drug abuse, including alcohol and prescription drugs can induce symptomatology which resembles mental illness. This can occur both in the intoxicated state and also during the withdrawal state. In some cases these substance induced psychiatric disorders can persist long after detoxification, such as prolonged psychosis or depression after amphetamine or cocaine abuse. A protracted withdrawal syndrome can also occur with symptoms persisting for months after cessation of use. Benzodiazepines are the most notable drug for inducing prolonged withdrawal effects with symptoms sometimes persisting for years after cessation of use. Abuse of hallucinogens can trigger delusional and other psychotic phenomena long after cessation of use and cannabis may trigger panic attacks during intoxication and with use it may cause a state similar to dysthymia. Severe anxiety and depression are commonly induced by sustained alcohol abuse which in most cases abates with prolonged abstinence. Even moderate alcohol sustained use may increase anxiety and depression levels in some individuals. In most cases these drug induced psychiatric disorders fade away with prolonged abstinence.
Drug abuse makes central nervous system (CNS) effects, which produce changes in mood, levels of awareness or perceptions and sensations. Most of these drugs also alter systems other than the CNS. Some of these are often thought of as being abused. Some drugs appear to be more likely to lead to uncontrolled use than others.
Traditionally, new pharmacotherapies are quickly adopted in primary care settings, however; drugs for substance abuse treatment have faced many barriers. Naltrexone, a drug originally marketed under the name “ReVia,” and now marketed in intramuscular formulation as “Vivitrol” or in oral formulation as a generic, is a medication approved for the treatment of alcohol dependence. This drug has reached very few patients. This may be due to a number of factors, including resistance by Addiction Medicine specialists and lack of resources.
The ability to recognize the signs of drug use or the symptoms of drug use in family members by parents and spouses has been affected significantly by the emergence of home drug test technology which helps identify recent use of common street and prescription drugs with near lab quality accuracy.
Epidemiology
The initiation of drug and alcohol use is most likely to occur during adolescence, and some experimentation with substances by older adolescents is common. For example, results from Monitoring the Future (2008), a nationwide study on rates of substance use, show that 47% of 12th graders report having used an illicit drug at some point in their lives . In 2009 in the United States about 21% of high school students have taken prescription drugs without a prescription. And earlier in 2002, the World health Organization estimated that around 140 million people were alcohol dependent and another 400 million suffered alcohol-related problems. Thankfully, the large majority of adolescents will phase out of drug use before it becomes problematic. Thus, although rates of overall use are high, the percentage of adolescents who meet criteria for substance abuse is significantly lower (close to 5%) . According to BBC, “Worldwide, the UN estimates there are more than 50 million regular users of morphine diacetate (heroin), cocaine and synthetic drugs.”
Total recorded alcohol per capita consumption (15+), in liters of pure alcohol.
History
APA, AMA, and NCDA
In 1932, the American Psychiatric Association created a definition that used legality, social acceptability, and cultural familiarity as qualifying factors:
…as a general rule, we reserve the term drug abuse to apply to the illegal, nonmedical use of a limited number of substances, most of them drugs, which have properties of altering the mental state in ways that are considered by social norms and defined by statute to be inappropriate, undesirable, harmful, threatening, or, at minimum, culture-alien.”
In 1966, the American Medical Association’s Committee on Alcoholism and Addiction defined abuse of stimulants (amphetamines, primarily) in terms of ‘medical supervision’:
…’use’ refers to the proper place of stimulants in medical practice; ‘misuse’ applies to the physician’s role in initiating a potentially dangerous course of therapy; and ‘abuse’ refers to self-administration of these drugs without medical supervision and particularly in large doses that may lead to psychological dependency, tolerance and abnormal behavior.
In 1973 the National Commission on Marijuana and Drug Abuse stated:
…drug abuse may refer to any type of drug or chemical without regard to its pharmacologic actions. It is an eclectic concept having only one uniform connotation: societal disapproval. … The Commission believes that the term drug abuse must be deleted from official pronouncements and public policy dialogue. The term has no functional utility and has become no more than an arbitrary codeword for that drug use which is presently considered wrong.
DSM
In the first edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (published in 1952) grouped alcohol and drug abuse under Sociopathic Personality Disturbances, which were thought to be symptoms of deeper psychological disorders or moral weakness.
The third edition, published in 1980, was the first to recognize substance abuse (including drug abuse) and substance dependence as conditions separate from substance abuse alone, bringing in social and cultural factors. The definition of dependence emphasised tolerance to drugs, and withdrawal from them as key components to diagnosis, whereas abuse was defined as “problematic use with social or occupational impairment” but without withdrawal or tolerance.
In 1987 the DSM-IIIR category “psychoactive substance abuse,” which includes former concepts of drug abuse is defined as “a maladaptive pattern of use indicated by…continued use despite knowledge of having a persistent or recurrent social, occupational, psychological or physical problem that is caused or exacerbated by the use (or by) recurrent use in situations in which it is physically hazardous.” It is a residual category, with dependence taking precedence when applicable. It was the first definition to give equal weight to behavioural and physiological factors in diagnosis.
By 1988, the DSM-IV defines substance dependence as “a syndrome involving compulsive use, with or without tolerance and withdrawal”; whereas substance abuse is “problematic use without compulsive use, significant tolerance, or withdrawal.” Substance abuse can be harmful to your health and may even be deadly in certain scenarios
By 1994, The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) issued by the American Psychiatric Association, the DSM-IV-TR, defines substance dependence as “when an individual persists in use of alcohol or other drugs despite problems related to use of the substance, substance dependence may be diagnosed.” followed by criteria for the diagnose
DSM-IV-TR defines substance abuse as:
A. A maladaptive pattern of substance use leading to clinically significant impairment or distress, as manifested by one (or more) of the following, occurring within a 12-month period:
Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home (e.g., repeated absences or poor work performance related to substance use; substance-related absences, suspensions or expulsions from school; neglect of children or household)
Recurrent substance use in situations in which it is physically hazardous (e.g., driving an automobile or operating a machine when impaired by substance use)
Recurrent substance-related legal problems (e.g., arrests for substance-related disorderly conduct)
Continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance (e.g., arguments with spouse about consequences of intoxication, physical fights)
B. The symptoms have never met the criteria for Substance Dependence for this class of substance.
The fifth edition of the DSM (DSM-5), planned for release in 2013, is likely to have this terminology revisited yet again. Under consideration is a transition from the abuse/dependence terminology. At the moment, abuse is seen as an early form or less hazardous form of the disease characterized with the dependence criteria. However, the APA’s ‘dependence’ term, as noted above, does not mean that physiologic dependence is present but rather means that a disease state is present, one that most would likely refer to as an addicted state. Many involved recognize that the terminology has often led to confusion, both within the medical community and with the general public. The American Psychiatric Association requests input as to how the terminology of this illness should be altered as it moves forward with DSM-5 discussion.
Society and culture
Legal approaches
Most governments have designed legislation to criminalize certain types of drug use. These drugs are often called “illegal drugs” but generally what is illegal is their unlicensed production, distribution, and possession. These drugs are also called “controlled substances”. Even for simple possession, legal punishment can be quite severe (including the death penalty in some countries). Laws vary across countries, and even within them, and have fluctuated widely throughout history.
Attempts by government-sponsored drug control policy to interdict drug supply and eliminate drug abuse have been largely unsuccessful. In spite of the huge efforts by the U.S., drug supply and purity has reached an all time high, with the vast majority of resources spent on interdiction and law enforcement instead of public health. In the United States, the number of nonviolent drug offenders in prison exceeds by 100,000 the total incarcerated population in the EU, despite the fact that the EU has 100 million more citizens.
Despite drug legislation (or perhaps because of it), large, organized criminal drug cartels operate worldwide. Advocates of decriminalization argue that drug prohibition makes drug dealing a lucrative business, leading to much of the associated criminal activity.
Cost
The UK Home Office estimated that the social and economic cost of drug abuse to the UK economy in terms of crime, absenteeism and sickness is in excess of £20 billion a year.
However, it does not estimate what portion of those crimes are unintended consequences of drug prohibition (crimes to sustain expensive drug consumption, risky production and dangerous distribution), nor what is the cost of enforcement. Those aspects are necessary for a full analysis of the economics of prohibition.
The Home Office has a recent history of taking a hard line on controlled drugs, including those with no known fatalities and even medical benefits, in direct opposition to the scientific community.
Treatment
Treatment for binge drinking and other forms of substance abuse is critical for many around the world. Often a formal intervention is necessary to convince the substance abuser to submit to any form of treatment. Behavioral interventions and medications exist that have helped many people reduce, or discontinue, their substance abuse. From the applied behavior analysis literature, the behavioral psychology literature, and from randomized clinical trials, several evidenced based interventions have emerged:
- Behavioral Marital Therapy
- Motivational Interviewing
- Community Reinforcement Approach
- Exposure therapy
- Contingency Management
- Pharmacological therapy
A number of medications have been approved for the treatment of substance abuse. These include replacement therapies such as buprenorphine and methadone as well as antagonist medications like disulfiram and naltrexone in either short acting, or the newer long acting form (under the brand name Vivitrol). Several other medications, often ones originally used in other contexts, have also been shown to be effective including bupropion (Zyban or Wellbutrin), Modafinil (Provigil) and more.
In children and adolescents, cognitive behavioral therapy (CBT) and family therapy currently have the most research evidence for the treatment of substance abuse problems. These treatments can be administered in a variety of different formats, each of which has varying levels of research support
It has been suggested that social skills training adjunctive to inpatient treatment of alcohol dependence is probably efficacious.