Clinical psychology is a branch of psychology that focuses on understanding, diagnosing, and treating mental and emotional disorders. It encompasses a wide range of principles and practices that are essential for providing effective psychological interventions to individuals in need. These principles and practices are based on scientific research and are constantly evolving to keep up with the changing needs of society. In this introductory guide, we will explore the fundamental principles and practices involved in the field of clinical psychology and how they are applied to promote mental health and well-being.
Clinical psychology is an integration of science, theory and clinical knowledge for the purpose of understanding, preventing, and relieving psychologically based distress or dysfunction and to promote subjective well-being and personal development. Central to its practice are psychological assessment, clinical formulation and psychotherapy, although clinical psychologists also engage in research, teaching, consultation, forensic testimony, and program development and administration. In many countries, clinical psychology is a regulated mental health profession.
The field is often considered to have begun in 1896 with the opening of the first psychological clinic at the University of Pennsylvania by Lightner Witmer. In the first half of the 20th century, clinical psychology was focused on psychological assessment, with little attention given to treatment. This changed after the 1940s when World War II resulted in the need for a large increase in the number of trained clinicians. Since that time, three main educational models have developed in the USA—the Ph.D. Clinical Science model (heavily focused on research), the Ph.D. science-practitioner model (integrating research and practice), and the Psy.D. practitioner-scholar model (focusing on clinical practice). In the UK the Clinical Psychology Doctorate falls between the latter two of these models, whilst in much of mainland Europe the training is at masters level and predominantly psychotherapeutic. Clinical psychologists are expert in providing psychotherapy, and generally train within four primary theoretical orientations—psychodynamic, humanistic, behavior therapy/ cognitive behavioral, and systems or family therapy.
History
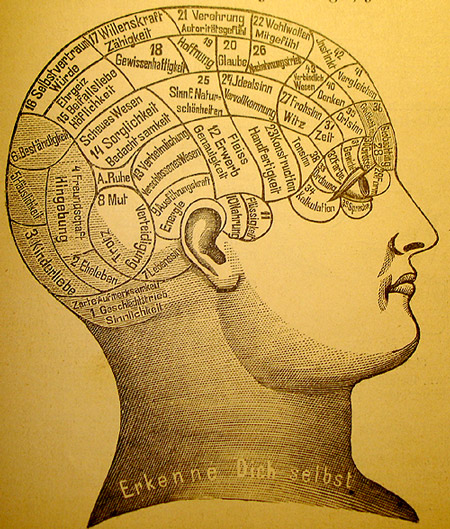
Many 18th c. treatments for psychological distress were based on pseudo-scientific ideas, such as Phrenology.
The earliest recorded approaches to assess and treat mental distress were a combination of religious, magical and/or medical perspectives. Early examples of such physicians included Patañjali, Padmasambhava, Rhazes, Avicenna, and Rumi. In the early 19th century, one approach to study mental conditions and behavior was using phrenology, the study of personality by examining the shape of the skull. Other popular treatments at that time included the study of the shape of the face (physiognomy) and Mesmer’s treatment for mental conditions using magnets (mesmerism). Spiritualism and Phineas Quimby’s “mental healing” were also popular.
While the scientific community eventually came to reject all of these methods for treating mental illness, academic psychologists also were not concerned with serious forms of mental illness. The study of mental illness was already being done in the developing fields of psychiatry and neurology within the asylum movement. It was not until the end of the 19th century, around the time when Sigmund Freud was first developing his “talking cure” in Vienna, that the first scientific application of clinical psychology began.
Early clinical psychology
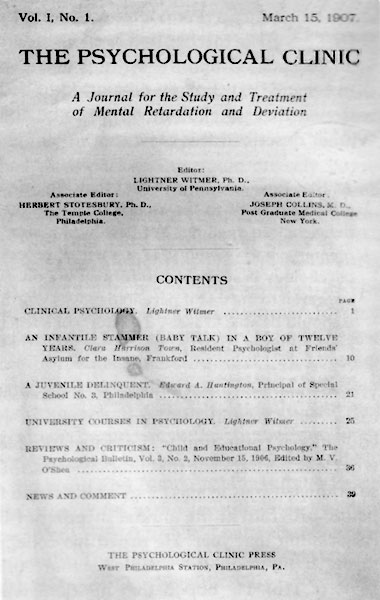
Cover of The Psychological Clinic, the first journal of clinical psychology, published in 1907 by Lightner Witmer
By the second half of the 1800s, the scientific study of psychology was becoming well established in university laboratories. Although there were a few scattered voices calling for an applied psychology, the general field looked down upon this idea and insisted on “pure” science as the only respectable practice. This changed when Lightner Witmer (1867–1956), a past student of Wundt and head of the psychology department at the University of Pennsylvania, agreed to treat a young boy who had trouble with spelling. His successful treatment was soon to lead to Witmer’s opening of the first psychological clinic at Penn in 1896, dedicated to helping children with learning disabilities. Ten years later in 1907, Witmer was to found the first journal of this new field, The Psychological Clinic, where he coined the term “clinical psychology”, defined as “the study of individuals, by observation or experimentation, with the intention of promoting change”. The field was slow to follow Witmer’s example, but by 1914, there were 26 similar clinics in the U.S.
Even as clinical psychology was growing, working with issues of serious mental distress remained the domain of psychiatrists and neurologists. However, clinical psychologists continued to make inroads into this area due to their increasing skill at psychological assessment. Psychologists’ reputation as assessment experts became solidified during World War I with the development of two intelligence tests, Army Alpha and Army Beta (testing verbal and nonverbal skills, respectively), which could be used with large groups of recruits. Due in large part to the success of these tests, assessment was to become the core discipline of clinical psychology for the next quarter century, when another war would propel the field into treatment.
Early professional organizations
The field began to organize under the name “clinical psychology” in 1917 with the founding of the American Association of Clinical Psychology. This only lasted until 1919, after which the American Psychological Association (founded by G. Stanley Hall in 1892) developed a section on Clinical Psychology, which offered certification until 1927. Growth in the field was slow for the next few years when various unconnected psychological organizations came together as the American Association of Applied Psychology in 1930, which would act as the primary forum for psychologists until after World War II when the APA reorganized. In 1945, the APA created what is now called Division 12, its division of clinical psychology, which remains a leading organization in the field. Psychological societies and associations in other English-speaking countries developed similar divisions, including in Britain, Canada, Australia and New Zealand.
World War II and the integration of treatment
When World War II broke out, the military once again called upon clinical psychologists. As soldiers began to return from combat, psychologists started to notice symptoms of psychological trauma labeled “shell shock” (eventually to be termed posttraumatic stress disorder) that were best treated as soon as possible. Because physicians (including psychiatrists) were over-extended in treating bodily injuries, psychologists were called to help treat this condition. At the same time, female psychologists (who were excluded from the war effort) formed the National Council of Women Psychologists with the purpose of helping communities deal with the stresses of war and giving young mothers advice on child rearing. After the war, the Veterans Administration in the U.S. made an enormous investment to set up programs to train doctoral-level clinical psychologists to help treat the thousands of veterans needing care. As a consequence, the U.S. went from having no formal university programs in clinical psychology in 1946 to over half of all Ph.D.s in psychology in 1950 being awarded in clinical psychology.
WWII helped bring dramatic changes to clinical psychology, not just in America but internationally as well. Graduate education in psychology began adding psychotherapy to the science and research focus based on the 1947 scientist-practitioner model, known today as the Boulder Model, for Ph.D. programs in clinical psychology. Clinical psychology in Britain developed much like in the U.S. after WWII, specifically within the context of the National Health Service with qualifications, standards, and salaries managed by the British Psychological Society.
Development of the Doctor of Psychology degree
By the 1960s, psychotherapy had become imbedded within clinical psychology, but for many the Ph.D. educational model did not offer the necessary training for those interested in practice rather than research. There was a growing argument that said the field of psychology in the U.S. had developed to a degree warranting explicit training in clinical practice. The concept of a practice-oriented degree was debated in 1965 and narrowly gained approval for a pilot program at the University of Illinois starting in 1968. Several other similar programs were instituted soon after, and in 1973, at the Vail Conference on Professional Training in Psychology, the practitioner–scholar model of clinical psychology—or Vail Model—resulting in the Doctor of Psychology (Psy.D.) degree was recognized. Although training would continue to include research skills and a scientific understanding of psychology, the intent would be to produce highly trained professionals, similar to programs in medicine, dentistry, and law. The first program explicitly based on the Psy.D. model was instituted at Rutgers University. Today, about half of all American graduate students in clinical psychology are enrolled in Psy.D. programs.
A changing profession
Since the 1970s, clinical psychology has continued growing into a robust profession and academic field of study. Although the exact number of practicing clinical psychologists is unknown, it is estimated that between 1974 and 1990, the number in the U.S. grew from 20,000 to 63,000. Clinical psychologists continue to be experts in assessment and psychotherapy while expanding their focus to address issues of gerontology, sports, and the criminal justice system to name a few. One important field is health psychology, the fastest-growing employment setting for clinical psychologists in the past decade. Other major changes include the impact of managed care on mental health care; an increasing realization of the importance of knowledge relating to multicultural and diverse populations; and emerging privileges to prescribe psychotropic medication.
Professional practice
Clinical psychologists engage in a wide range of activities. Some focus solely on research into the assessment, treatment, or cause of mental illness and related conditions. Some teach, whether in a medical school or hospital setting, or in an academic department (e.g., psychology department) at an institution of higher education. The majority of clinical psychologists engage in some form of clinical practice, with professional services including psychological assessment, provision of psychotherapy, development and administration of clinical programs, and forensics (e.g., providing expert testimony in a legal proceeding.
In clinical practice, clinical psychologists may work with individuals, couples, families, or groups in a variety of settings, including private practices, hospitals, mental health organizations, schools, businesses, and non-profit agencies. Clinical psychologists who provide clinical services may also choose to specialize. Some specializations are codified and credentialed by regulatory agencies within the country of practice. In the United States such specializations are credentialed by the American Board of Professional Psychology (ABPP).
Training and certification to practice

The University of Pennsylvania was the first to offer formal education in clinical psychology.
Clinical psychologists study a generalist program in psychology plus postgraduate training and/or clinical placement and supervision. The length of training differs across the world, ranging from four years plus post-Bachelors supervised practice to a doctorate of three to six years which combines clinical placement. In the USA, about half of all clinical psychology graduate students are being trained in Ph.D. programs—a model that emphasizes research—with the other half in Psy.D. programs, which has more focus on practice (similar to professional degrees for medicine and law). Both models are accredited by the American Psychological Association and many other English-speaking psychological societies. A smaller number of schools offer accredited programs in clinical psychology resulting in a Masters degree, which usually take two to three years post-Bachelors.
In the U.K., clinical psychologists undertake a Doctor of Clinical Psychology (D.Clin.Psych.), which is a practitioner doctorate with both clinical and research components. This is a three-year full-time salaried program sponsored by the National Health Service (NHS) and based in universities and the NHS. Entry into these programs is highly competitive, and requires at least a three-year undergraduate degree in psychology plus some form of experience, usually in either the NHS as an Assistant Psychologist or in academia as a Research Assistant. It is not unusual for applicants to apply several times before being accepted onto a training course as only about one-fifth of applicants are accepted each year. These clinical psychology doctoral degrees are accredited by the British Psychological Society and the Health Professions Council (HPC). The HPC is the statutory regulator for practitioner psychologists in the UK. Those who successfully complete clinical psychology doctoral degrees are eligible to apply for registration with the HPC as a clinical psychologist.
The practice of clinical psychology requires a license in the United States, Canada, the United Kingdom, and many other countries. Although each of the U.S. states is somewhat different in terms of requirements and licenses, there are three common elements:
- Graduation from an accredited school with the appropriate degree
- Completion of supervised clinical experience or internship
- Passing a written examination and, in some states, an oral examination
All U.S. state and Canadian province licensing boards are members of the Association of State and Provincial Psychology Boards (ASPPB) which created and maintains the Examination for Professional Practice in Psychology (EPPP). Many states require other examinations in addition to the EPPP, such as a jurisprudence (i.e. mental health law) examination and/or an oral examination. Most states also require a certain number of continuing education credits per year in order to renew a license, which can be obtained though various means, such as taking audited classes and attending approved workshops. Clinical psychologists require the Psychologist license to practice, although licenses can be obtained with a masters-level degree, such as Marriage and Family Therapist (MFT), Licensed Professional Counselor (LPC), and Licensed Psychological Associate (LPA).
In the U.K. registration as a clinical psychologist with the Health Professions Council (HPC) is necessary. The HPC is the statutory regulator for practitioner psychologists in the U.K. In the U.K. the following titles are restricted by law “registered psychologist” and “practitioner psychologist”; in addition the specialist title “clinical psychologist” is also restricted by law.
Assessment
An important area of expertise for many clinical psychologists is psychological assessment, and there are indications that as many as 91% of psychologists engage in this core clinical practice. Such evaluation is usually done in service to gaining insight into and forming hypotheses about psychological or behavioral problems. As such, the results of such assessments are usually used to create generalized impressions (rather than diagnoses) in service to informing treatment planning. Methods include formal testing measures, interviews, reviewing past records, clinical observation, and physical examination.
Measurement domains
There exist hundreds of various assessment tools, although only a few have been shown to have both high validity (i.e., test actually measures what it claims to measure) and reliability (i.e., consistency). These measures generally fall within one of several categories, including the following:
- Intelligence & achievement tests – These tests are designed to measure certain specific kinds of cognitive functioning (often referred to as IQ) in comparison to a norming-group. These tests, such as the WISC-IV, attempt to measure such traits as general knowledge, verbal skill, memory, attention span, logical reasoning, and visual/spatial perception. Several tests have been shown to predict accurately certain kinds of performance, especially scholastic.
- Personality tests – Tests of personality aim to describe patterns of behavior, thoughts, and feelings. They generally fall within two categories: objective and projective. Objective measures, such as the MMPI, are based on restricted answers—such as yes/no, true/false, or a rating scale—which allow for computation of scores that can be compared to a normative group. Projective tests, such as the Rorschach inkblot test, allow for open-ended answers, often based on ambiguous stimuli, presumably revealing non-conscious psychological dynamics.
- Neuropsychological tests – Neuropsychological tests consist of specifically designed tasks used to measure psychological functions known to be linked to a particular brain structure or pathway. They are typically used to assess impairment after an injury or illness known to affect neurocognitive functioning, or when used in research, to contrast neuropsychological abilities across experimental groups.
- Clinical observation – Clinical psychologists are also trained to gather data by observing behavior. The clinical interview is a vital part of assessment, even when using other formalized tools, which can employ either a structured or unstructured format. Such assessment looks at certain areas, such as general appearance and behavior, mood and affect, perception, comprehension, orientation, insight, memory, and content of communication. One psychiatric example of a formal interview is the mental status examination, which is often used in psychiatry as a screening tool for treatment or further testing.
Diagnostic impressions
Published by the American Psychiatric Association, the Diagnostic and Statistical Manual of Mental Disorders (DSM) provides a common language and standard criteria for the classification of mental disorders.
After assessment, clinical psychologists often provide a diagnostic impression. Many countries use the International Statistical Classification of Diseases and Related Health Problems (ICD-10) while the U.S. most often uses the Diagnostic and Statistical Manual of Mental Disorders. Both are nosological systems that largely assume categorical disorders diagnosed through the application of sets of criteria including symptoms and signs.
Several new models are being discussed, including a “dimensional model” based on empirically validated models of human differences (such as the five factor model of personality) and a “psychosocial model”, which would take changing, intersubjective states into greater account. The proponents of these models claim that they would offer greater diagnostic flexibility and clinical utility without depending on the medical concept of illness. However, they also admit that these models are not yet robust enough to gain widespread use, and should continue to be developed.
Clinical psychologists do not tend to diagnose, but rather use formulation—an individualized map of the difficulties that the patient or client faces, encompassing predisposing, precipitating and perpetuating (maintaining) factors.
Clinical v. mechanical prediction
Clinical assessment can be characterized as a prediction problem where the purpose of assessment is to make inferences (predictions) about past, present, or future behavior. For example, many therapy decisions are made on the basis of what a clinician expects will help a patient make therapeutic gains. Once observations have been collected (e.g., psychological test results, diagnostic impressions, clinical history, X-ray, etc.), there are two mutually exclusive ways to combine those sources of information to arrive at a decision, diagnosis, or prediction. One way is to combine the data in an algorithmic, or “mechanical” fashion. Mechanical prediction methods are simply a mode of combination of data to arrive at a decision/prediction of behavior (e.g., treatment response). Mechanical prediction does not preclude any type of data from being combined; it can incorporate clinical judgments, properly coded, in the algorithm. The defining characteristic is that, once the data to be combined is given, the mechanical approach will make a prediction that is 100% reliable. That is, it will make exactly the same prediction for exactly the same data every time. Clinical prediction, on the other hand, does not guarantee this, as it depends on the decision-making processes of the clinician making the judgment, their current state of mind, and knowledge base.
What has come to be called the “clinical versus statistical prediction” debate was first described in detail in 1954 by Paul Meehl, where he explored the claim that mechanical (formal, algorithmic) methods of data combination could outperform clinical (e.g., subjective, informal, “in the clinician’s head”) methods when such combinations are used to arrive at a prediction of behavior. Meehl concluded that mechanical modes of combination performed as well or better than clinical modes. Subsequent meta-analyses of studies that directly compare mechanical and clinical predictions have born out Meehl’s 1954 conclusions. A 2009 survey of practicing clinical psychologists found that clinicians almost exclusively use their clinical judgment to make behavioral predictions for their patients, including diagnosis and prognosis.
Intervention
Psychotherapy involves a formal relationship between professional and client—usually an individual, couple, family, or small group—that employs a set of procedures intended to form a therapeutic alliance, explore the nature of psychological problems, and encourage new ways of thinking, feeling, or behaving.
Clinicians have a wide range of individual interventions to draw from, often guided by their training—for example, a cognitive behavioral therapy (CBT) clinician might use worksheets to record distressing cognitions, a psychoanalyst might encourage free association, while a psychologist trained in Gestalt techniques might focus on immediate interactions between client and therapist. Clinical psychologists generally seek to base their work on research evidence and outcome studies as well as on trained clinical judgment. Although there are literally dozens of recognized therapeutic orientations, their differences can often be categorized on two dimensions: insight vs. action and in-session vs. out-session.
- Insight – emphasis is on gaining greater understanding of the motivations underlying one’s thoughts and feelings (e.g. psychodynamic therapy)
- Action – focus is on making changes in how one thinks and acts (e.g. solution focused therapy, cognitive behavioral therapy)
- In-session – interventions center on the here-and-now interaction between client and therapist (e.g. humanistic therapy, Gestalt therapy)
- Out-session – a large portion of therapeutic work is intended to happen outside of session (e.g. bibliotherapy, rational emotive behavior therapy)
The methods used are also different in regards to the population being served as well as the context and nature of the problem. Therapy will look very different between, say, a traumatized child, a depressed but high-functioning adult, a group of people recovering from substance dependence, and a ward of the state suffering from terrifying delusions. Other elements that play a critical role in the process of psychotherapy include the environment, culture, age, cognitive functioning, motivation, and duration (i.e. brief or long-term therapy).
Four main schools
Many clinical psychologists are integrative or eclectic and draw from the evidence base across different models of therapy in an integrative way, rather than using a single specific model.
In the UK, clinical psychologists have to show competence in at least two models of therapy, including CBT, to gain their doctorate. The British Psychological Society Division of Clinical Psychology has been vocal about the need to follow the evidence base rather than being wedded to a single model of therapy.
In the USA, intervention applications and research are dominated in training and practice by essentially four major schools of practice: psychodynamic, humanistic, behavioral/cognitive behavioral, and systems or family therapy.
Psychodynamic
The psychodynamic perspective developed out of the psychoanalysis of Sigmund Freud. The core object of psychoanalysis is to make the unconscious conscious—to make the client aware of his or her own primal drives (namely those relating to sex and aggression) and the various defenses used to keep them in check. The essential tools of the psychoanalytic process are the use of free association and an examination of the client’s transference towards the therapist, defined as the tendency to take unconscious thoughts or emotions about a significant person (e.g. a parent) and “transfer” them onto another person. Major variations on Freudian psychoanalysis practiced today include self psychology, ego psychology, and object relations theory. These general orientations now fall under the umbrella term psychodynamic psychology, with common themes including examination of transference and defenses, an appreciation of the power of the unconscious, and a focus on how early developments in childhood have shaped the client’s current psychological state.
Humanistic
Humanistic psychology was developed in the 1950s in reaction to both behaviorism and psychoanalysis, largely due to the person-centered therapy of Carl Rogers (often referred to as Rogerian Therapy) and existential psychology developed by Viktor Frankl and Rollo May. Rogers believed that a client needed only three things from a clinician to experience therapeutic improvement—congruence, unconditional positive regard, and empathetic understanding. By using phenomenology, intersubjectivity and first-person categories, the humanistic approach seeks to get a glimpse of the whole person and not just the fragmented parts of the personality. This aspect of holism links up with another common aim of humanistic practice in clinical psychology, which is to seek an integration of the whole person, also called self-actualization. From 1980, Hans-Werner Gessmann integrated the ideas of humanistic psychology into group psychotherapy as humanistic psychodrama. According to humanistic thinking, each individual person already has inbuilt potentials and resources that might help them to build a stronger personality and self-concept. The mission of the humanistic psychologist is to help the individual employ these resources via the therapeutic relationship.
Behavioral and cognitive behavioral
Cognitive behavioral therapy (CBT) developed from the combination of cognitive therapy and rational emotive behavior therapy, both of which grew out of cognitive psychology and behaviorism. CBT is based on the theory that how we think (cognition), how we feel (emotion), and how we act (behavior) are related and interact together in complex ways. In this perspective, certain dysfunctional ways of interpreting and appraising the world (often through schemas or beliefs) can contribute to emotional distress or result in behavioral problems. The object of many cognitive behavioral therapies is to discover and identify the biased, dysfunctional ways of relating or reacting and through different methodologies help clients transcend these in ways that will lead to increased well-being. There are many techniques used, such as systematic desensitization, socratic questioning, and keeping a cognition observation log. Modified approaches that fall into the category of CBT have also developed, including dialectic behavior therapy and mindfulness-based cognitive therapy.
Behavior therapy is a rich tradition. It is well researched with a strong evidence base. Its roots are in behaviorism. In behavior therapy, environmental events predict the way we think and feel. Our behavior sets up conditions for the environment to feedback back on it. Sometimes the feedback leads the behavior to increase- reinforcement and sometimes the behavior decreases- punishment. Oftentimes behavior therapists are called applied behavior analysis. They have studied many areas from developmental disabilities to depression and anxiety disorders. In the area of mental health and addictions a recent article looked at APA’s list for well established and promising practices and found a considerable number of them based on the principles of operant and respondent conditioning. Multiple assessment techniques have come from this approach including functional analysis (psychology), which has found a strong focus in the school system. In addition, multiple intervention programs have come from this tradition including community reinforcement approach for treating addictions, acceptance and commitment therapy, functional analytic psychotherapy, including dialectic behavior therapy and behavioral activation. In addition, specific techniques such as contingency management and exposure therapy have come from this tradition.
Systems or family therapy
Systems or family therapy works with couples and families, and emphasizes family relationships as an important factor in psychological health. The central focus tends to be on interpersonal dynamics, especially in terms of how change in one person will affect the entire system. Therapy is therefore conducted with as many significant members of the “system” as possible. Goals can include improving communication, establishing healthy roles, creating alternative narratives, and addressing problematic behaviors.
Other therapeutic perspectives
There exist dozens of recognized schools or orientations of psychotherapy—the list below represents a few influential orientations not given above. Although they all have some typical set of techniques practitioners employ, they are generally better known for providing a framework of theory and philosophy that guides a therapist in his or her working with a client.
- Existential – Existential psychotherapy postulates that people are largely free to choose who we are and how we interpret and interact with the world. It intends to help the client find deeper meaning in life and to accept responsibility for living. As such, it addresses fundamental issues of life, such as death, aloneness, and freedom. The therapist emphasizes the client’s ability to be self-aware, freely make choices in the present, establish personal identity and social relationships, create meaning, and cope with the natural anxiety of living.
- Gestalt – Gestalt therapy was primarily founded by Fritz Perls in the 1950s. This therapy is perhaps best known for using techniques designed to increase self-awareness, the best-known perhaps being the “empty chair technique.” Such techniques are intended to explore resistance to “authentic contact”, resolve internal conflicts, and help the client complete “unfinished business”.
- Postmodern – Postmodern psychology says that the experience of reality is a subjective construction built upon language, social context, and history, with no essential truths. Since “mental illness” and “mental health” are not recognized as objective, definable realities, the postmodern psychologist instead sees the goal of therapy strictly as something constructed by the client and therapist. Forms of postmodern psychotherapy include narrative therapy, solution-focused therapy, and coherence therapy.
- Transpersonal – The transpersonal perspective places a stronger focus on the spiritual facet of human experience. It is not a set of techniques so much as a willingness to help a client explore spirituality and/or transcendent states of consciousness. It also is concerned with helping clients achieve their highest potential.
- Multiculturalism – Although the theoretical foundations of psychology are rooted in European culture, there is a growing recognition that there exist profound differences between various ethnic and social groups and that systems of psychotherapy need to take those differences into greater consideration. Further, the generations following immigrant migration will have some combination of two or more cultures—with aspects coming from the parents and from the surrounding society—and this process of acculturation can play a strong role in therapy (and might itself be the presenting problem). Culture influences ideas about change, help-seeking, locus of control, authority, and the importance of the individual versus the group, all of which can potentially clash with certain givens in mainstream psychotherapeutic theory and practice. As such, there is a growing movement to integrate knowledge of various cultural groups in order to inform therapeutic practice in a more culturally sensitive and effective way.
- Feminism – Feminist therapy is an orientation arising from the disparity between the origin of most psychological theories (which have male authors) and the majority of people seeking counseling being female. It focuses on societal, cultural, and political causes and solutions to issues faced in the counseling process. It openly encourages the client to participate in the world in a more social and political way.
- Positive psychology – Positive psychology is the scientific study of human happiness and well-being, which started to gain momentum in 1998 due to the call of Martin Seligman, then president of the APA. The history of psychology shows that the field has been primarily dedicated to addressing mental illness rather than mental wellness. Applied positive psychology’s main focus, therefore, is to increase one’s positive experience of life and ability to flourish by promoting such things as optimism about the future, a sense of flow in the present, and personal traits like courage, perseverance, and altruism. There is now preliminary empirical evidence to show that by promoting Seligman’s three components of happiness—positive emotion (the pleasant life), engagement (the engaged life), and meaning (the meaningful life)—positive therapy can decrease clinical depression.
Integration
In the last couple of decades, there has been a growing movement to integrate the various therapeutic approaches, especially with an increased understanding of cultural, gender, spiritual, and sexual-orientation issues. Clinical psychologists are beginning to look at the various strengths and weaknesses of each orientation while also working with related fields, such as neuroscience, behavioral genetics, evolutionary biology, and psychopharmacology. The result is a growing practice of eclecticism, with psychologists learning various systems and the most efficacious methods of therapy with the intent to provide the best solution for any given problem.
Professional ethics
The field of clinical psychology in most countries is strongly regulated by a code of ethics. In the U.S., professional ethics are largely defined by the APA Code of Conduct, which is often used by states to define licensing requirements. The APA Code generally sets a higher standard than that which is required by law as it is designed to guide responsible behavior, the protection of clients, and the improvement of individuals, organizations, and society. The Code is applicable to all psychologists in both research and applied fields.
The APA Code is based on five principles: Beneficence and Nonmaleficence, Fidelity and Responsibility, Integrity, Justice, and Respect for People’s Rights and Dignity. Detailed elements address how to resolve ethical issues, competence, human relations, privacy and confidentiality, advertising, record keeping, fees, training, research, publication, assessment, and therapy.
In the UK the British Psychological Society has published a Code of Conduct and Ethics for clinical psychologists. This has four key areas: Respect, Competence, Responsibility and Integrity. Other European professional organisations have similar codes of conduct and ethics.
Comparison with other mental health professions
Psychiatry
Fluoxetine hydrochloride, branded by Lilly as Prozac, is a antidepressant drug prescribed by physicians, psychiatrists, and some nurses.
Although clinical psychologists and psychiatrists can be said to share a same fundamental aim—the alleviation of mental distress—their training, outlook, and methodologies are often quite different. Perhaps the most significant difference is that psychiatrists are licensed physicians. As such, psychiatrists often use the medical model to assess psychological problems (i.e., those they treat are seen as patients with an illness) and rely on psychotropic medications as the chief method of addressing the illness—although many also employ psychotherapy as well. Psychiatrists and medical psychologists (who are clinical psychologists that are also licensed to prescribe) are able to conduct physical examinations, order and interpret laboratory tests and EEGs, and may order brain imaging studies such as CT or CAT, MRI, and PET scanning.
Clinical psychologists generally do not prescribe medication, although there is a growing movement for psychologists to have prescribing privileges. These medical privileges require additional training and education. To date, medical psychologists may prescribe psychotropic medications in Guam, New Mexico, and Louisiana and military psychologists.
Counseling psychology
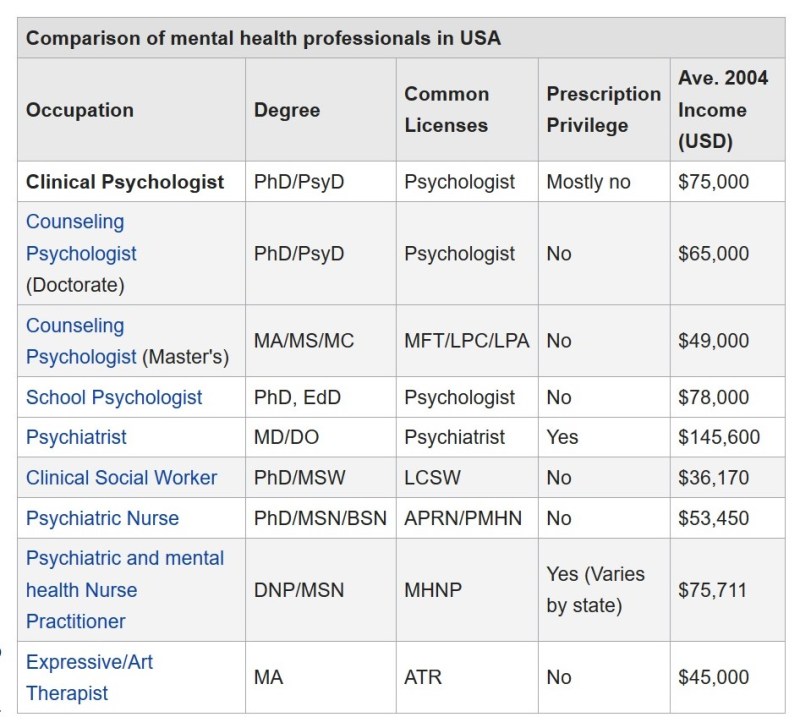
Counseling psychologists study and use many of the same interventions and tools as clinical psychologists, including psychotherapy and assessment. Traditionally, counseling psychologists help people with what might be considered normal or moderate psychological problems—such as the feelings of anxiety or sadness resulting from major life changes or events. Many counseling psychologists also receive specialized training in career assessment, group therapy, and relationship counseling, although some counseling psychologists also work with the more serious problems that clinical psychologists are trained for, such as dementia or psychosis.
There are fewer counseling psychology graduate programs than those for clinical psychology and they are more often housed in departments of education rather than psychology. The two professions can be found working in all the same settings but counseling psychologists are more frequently employed in university counseling centers compared to hospitals and private practice for clinical psychologists. There is considerable overlap between the two fields and distinctions between them continue to fade.
School psychology
School psychologists are primarily concerned with the academic, social, and emotional well-being of children and adolescents within a scholastic environment. In the U.K., they are known as “educational psychologists”. Like clinical (and counseling) psychologists, school psychologists with doctoral degrees are eligible for licensure as health service psychologists, and many work in private practice. Unlike clinical psychologists, they receive much more training in education, child development and behavior, and the psychology of learning. Common degrees include the Educational Specialist Degree (Ed.S.), Doctor of Philosophy (Ph.D.), and Doctor of Education (Ed.D.).
Traditional job roles for school psychologists employed in school settings have focused mainly on assessment of students to determine their eligibility for special education services in schools, and on consultation with teachers and other school professionals to design and carry out interventions on behalf of students. Other major roles also include offering individual and group therapy with children and their families, designing prevention programs (e.g. for reducing dropout), evaluating school programs, and working with teachers and administrators to help maximize teaching efficacy, both in the classroom and systemically.
Clinical social work
Social workers provide a variety of services, generally concerned with social problems, their causes, and their solutions. With specific training, clinical social workers may also provide psychological counseling (in the U.S. and Canada), in addition to more traditional social work. The Masters in Social Work in the U.S. is a two-year, sixty credit program that includes at least a one-year practicum (two years for clinicians).
Occupational therapy
Occupational therapy—often abbreviated OT—is the “use of productive or creative activity in the treatment or rehabilitation of physically, cognitively, or emotionally disabled people.” Most commonly, occupational therapists work with people with disabilities to enable them to maximize their skills and abilities. Occupational therapy practitioners are skilled professionals whose education includes the study of human growth and development with specific emphasis on the physical, emotional, psychological, sociocultural, cognitive and environmental components of illness and injury. They commonly work alongside clinical psychologists in settings such as inpatient and outpatient mental health, pain management clinics, eating disorder clinics, and child development services. OT’s use support groups, individual counseling sessions, and activity-based approaches to address psychiatric symptoms and maximize functioning in life activities.
Criticisms and controversies
Clinical psychology is a diverse field and there have been recurring tensions over the degree to which clinical practice should be limited to treatments supported by empirical research. Despite some evidence showing that all the major therapeutic orientations are about of equal effectiveness, there remains much debate about the efficacy of various forms treatment in use in clinical psychology.
It has been reported that clinical psychology has rarely allied itself with client groups and tends to individualize problems to the neglect of wider economic, political and social inequality issues that may not be the responsibility of the client. It has been argued that therapeutic practices are inevitably bound up with power inequalities, which can be used for good and bad. A critical psychology movement has argued that clinical psychology, and other professions making up a “psy complex”, often fail to consider or address inequalities and power differences and can play a part in the social and moral control of disadvantage, deviance and unrest.
An October 2009 editorial in the journal Nature suggests that a large number of clinical psychology practitioners in the United States consider scientific evidence to be “less important than their personal – that is, subjective – clinical experience.”
Click on the topics below to explore further: