Schizophrenia, a complex and chronic mental disorder, affects millions of people worldwide. It is characterized by a range of symptoms that can significantly impact an individual’s thoughts, emotions, and behavior. The condition can be challenging to diagnose and treat, leading to significant impairment in daily functioning and quality of life. In this article, we will explore the various symptoms of schizophrenia and the available treatment options to manage this debilitating illness. Understanding the signs and treatment options can help individuals and their loved ones to navigate this disorder and improve their overall well-being.

Cloth embroidered by a patient diagnosed with schizophrenia
Schizophrenia is a mental disorder characterized by a disintegration of thought processes and of emotional responsiveness. It most commonly manifests as auditory hallucinations, paranoid or bizarre delusions, or disorganized speech and thinking, and it is accompanied by significant social or occupational dysfunction. The onset of symptoms typically occurs in young adulthood, with a global lifetime prevalence of about 0.3–0.7%. Diagnosis is based on observed behavior and the patient’s reported experiences.
Genetics, early environment, neurobiology, and psychological and social processes appear to be important contributory factors; some recreational and prescription drugs appear to cause or worsen symptoms. Current research is focused on the role of neurobiology, although no single isolated organic cause has been found. The many possible combinations of symptoms have triggered debate about whether the diagnosis represents a single disorder or a number of discrete syndromes. Despite the etymology of the term from the Greek roots skhizein (σχίζειν, “to split”) and phrēn, phren- (φρήν, φρεν-; “mind”), schizophrenia does not imply a “split mind” and it is not the same as dissociative identity disorder—also known as “multiple personality disorder” or “split personality”—a condition with which it is often confused in public perception.
The mainstay of treatment is antipsychotic medication, which primarily suppresses dopamine, and sometimes serotonin, receptor activity. Psychotherapy and vocational and social rehabilitation are also important in treatment. In more serious cases—where there is risk to self and others—involuntary hospitalization may be necessary, although hospital stays are now shorter and less frequent than they were.
The disorder is thought mainly to affect cognition, but it also usually contributes to chronic problems with behavior and emotion. People with schizophrenia are likely to have additional (comorbid) conditions, including major depression and anxiety disorders; the lifetime occurrence of substance abuse is almost 50%. Social problems, such as long-term unemployment, poverty and homelessness, are common. The average life expectancy of people with the disorder is 12 to 15 years less than those without, the result of increased physical health problems and a higher suicide rate (about 5%).
Signs and symptoms
A person diagnosed with schizophrenia may experience hallucinations (most reported are hearing voices), delusions (often bizarre or persecutory in nature), and disorganized thinking and speech. The latter may range from loss of train of thought, to sentences only loosely connected in meaning, to incoherence known as word salad in severe cases. Social withdrawal, sloppiness of dress and hygiene, and loss of motivation and judgement are all common in schizophrenia. There is often an observable pattern of emotional difficulty, for example lack of responsiveness. Impairment in social cognition is associated with schizophrenia, as are symptoms of paranoia; social isolation commonly occurs. In one uncommon subtype, the person may be largely mute, remain motionless in bizarre postures, or exhibit purposeless agitation, all signs of catatonia.
Late adolescence and early adulthood are peak periods for the onset of schizophrenia, critical years in a young adult’s social and vocational development. In 40% of men and 23% of women diagnosed with schizophrenia the condition manifested itself before the age of 19. To minimize the developmental disruption associated with schizophrenia, much work has recently been done to identify and treat the prodromal (pre-onset) phase of the illness, which has been detected up to 30 months before the onset of symptoms. Those who go on to develop schizophrenia may experience transient or self-limiting psychotic symptoms and the non-specific symptoms of social withdrawal, irritability, dysphoria, and clumsiness during the prodromal phase.
Schneiderian classification

The term schizophrenia was coined by Eugen Bleuler.
The psychiatrist Kurt Schneider (1887–1967) listed the forms of psychotic symptoms that he thought distinguished schizophrenia from other psychotic disorders. These are called first-rank symptoms or Schneider’s first-rank symptoms, and they include delusions of being controlled by an external force; the belief that thoughts are being inserted into or withdrawn from one’s conscious mind; the belief that one’s thoughts are being broadcast to other people; and hearing hallucinatory voices that comment on one’s thoughts or actions or that have a conversation with other hallucinated voices. Although they have significantly contributed to the current diagnostic criteria, the specificity of first-rank symptoms has been questioned. A review of the diagnostic studies conducted between 1970 and 2005 found that they allow neither a reconfirmation nor a rejection of Schneider’s claims, and suggested that first-rank symptoms be de-emphasized in future revisions of diagnostic systems.
Positive and negative symptoms
Schizophrenia is often described in terms of positive and negative (or deficit) symptoms. Positive symptoms are those that most individuals do not normally experience but are present in people with schizophrenia. They can include delusions, disordered thoughts and speech, and tactile, auditory, visual, olfactory and gustatory hallucinations, typically regarded as manifestations of psychosis. Hallucinations are also typically related to the content of the delusional theme. Positive symptoms generally respond well to medication. Negative symptoms are deficits of normal emotional responses or of other thought processes, and respond less well to medication. They commonly include flat or blunted affect and emotion, poverty of speech (alogia), inability to experience pleasure (anhedonia), lack of desire to form relationships (asociality), and lack of motivation (avolition). Research suggests that negative symptoms contribute more to poor quality of life, functional disability, and the burden on others than do positive symptoms. People with prominent negative symptoms often have a history of poor adjustment before the onset of illness, and response to medication is often limited.
Causes of schizophrenia
The causes of schizophrenia have been the subject of much debate, with various factors proposed and discounted or modified. The language of schizophrenia research under the medical model is scientific. Such studies suggest that genetics, prenatal development, early environment, neurobiology and psychological and social processes are important contributory factors.
Current psychiatric research into the development of the disorder is often based on a neurodevelopmental model (proponents of which see schizophrenia as a syndrome.) However, schizophrenia is diagnosed on the basis of symptom profiles. Neural correlates do not provide sufficiently useful criteria. “Current research into schizophrenia has remained highly fragmented, much like the clinical presentation of the disease itself”.
Although no common cause of schizophrenia has been identified in all individuals diagnosed with the condition, currently most researchers and clinicians believe it results from a combination of both brain vulnerabilities (either inherited or acquired) and life events. This widely adopted approach is known as the ‘stress-vulnerability’ model, and much scientific debate now focuses on how much each of these factors contributes to the development and maintenance of schizophrenia.
Schizophrenia is most commonly first diagnosed during late adolescence or early adulthood, suggesting it is often the end process of childhood and adolescent development. There is on average a somewhat earlier onset for men than women, with the possible influence of the female hormone estrogen being one hypothesis and sociocultural influences another.
Genetics
Evidence suggests that genetic vulnerability and environmental factors can act in combination to result in diagnosis of schizophrenia. Research suggests that genetic vulnerability to schizophrenia is multifactorial, caused by interactions of several genes.
Both individual twin studies and meta-analyses of twin studies estimate the heritability of risk for schizophrenia to be approximately 80% (this refers to the proportion of variation between individuals in a population that is influenced by genetic factors, not the degree of genetic determination of individual risk). Concordance rates between monozygotic twins was close to 50%; whereas dizygotic twins was 17%. Adoption studies have also indicated a somewhat increased risk in those with a parent with schizophrenia even when raised apart. Studies suggest that the phenotype is genetically influenced but not genetically determined; that the variants in genes are generally within the range of normal human variation and have low risk associated with them each individually; and that some interact with each other and with environmental risk factors; and that they may not be specific to schizophrenia.
Some twin studies have found rates as low as 11.0%–13.8% among monozygotic twins, and 1.8%–4.1% among dizygotic twins, however. Tyronne Cannon reviewed the situation, stating: “Previous twin studies have reported estimates of broad heritability ranging from 0.41 to 0.87” Yet, in the “Pairs of Veteran Twins” study, for example, 338 pairs were schizophrenic with only 26 pairs concordant, and it was concluded in one report: “the role of the suggested genetic factor appears to be a limited one; 85 percent of the affected monozygotic pairs in the sample were discordant for schizophrenia”. In addition, some scientists criticize the methodology of the twin studies, and have argued that the genetic basis of schizophrenia is still largely unknown or open to different interpretations.
For example, although the concordance of schizophrenia occurrence in monozygotic twins has traditionally been used to estimate a genetic component to the illness, the results could be skewed because of environmental factors like a shared placenta
In fact, researchers, have used the phenomenon of ‘fetal programming’ to account for familial patterns in epidemiological studies. “Intra-uterine growth is a complex outcome that is influenced by a wide range of factors including fetal genotype, maternal physiology and behaviour as well as the function of that crucial interface—the placenta,” said one journal.
After reviewing techniques like: Genome Wide Association Studies; Single Nucleotide Polymorphisms and Copy Number Variations; the Nature journal reports: the basic observation is that, “You have this clear tangible phenomenon in which children resemble their parents”….”Despite what children get told in elementary school science we just don’t know how that works,” as Professor of ecology and evolutionary biology at Princeton, Leonid Kruglyak says (in reviewing hereditibility in general). It cites schizophrenia as a trait in which the genes have gone missing.
A great deal of effort has been put into molecular genetic studies of schizophrenia, which attempt to identify specific genes which may increase risk. A 2003 review of linkage studies listed seven genes as likely to increase risk for a later diagnosis of the disorder. Two recent reviews suggested that the evidence was strongest for two genes known as dysbindin (DTNBP1) and neuregulin (NRG1), and that a number of other genes (such as COMT, RGS4, PPP3CC, ZDHHC8, DISC1, and AKT1) showed some early promising results. Variations near the gene FXYD6 have also been associated with schizophrenia in the UK but not in Japan. In 2008, rs7341475 SNP of the reelin gene was associated with an increased risk of schizophrenia in women, but not in men. This female-specific association was replicated in several populations. Still another review found evidence that the protein phosphatase 2B (calcineurin) might be involved in susceptibility to schizophrenia.
The largest most comprehensive genetic study of its kind, involving tests of several hundred single nucleotide polymorphisms (SNPs) in nearly 1,900 individuals with schizophrenia or schizoaffective disorder and 2,000 comparison subjects, reported in 2008 that there was no evidence of any significant association between the disorders and any of 14 previously identified candidate genes (RGS4, DISC1, DTNBP1, STX7, TAAR6, PPP3CC, NRG1, DRD2, HTR2A, DAOA, AKT1, CHRNA7, COMT, and ARVCF). The statistical distributions suggested nothing more than chance variation. The authors concluded that the findings make it unlikely that common SNPs in these genes account for a substantial proportion of the genetic risk for schizophrenia, although small effects could not be ruled out.
The perhaps largest analysis of genetic associations in schizophrenia is with the SzGene database at the Schizophrenia Research Forum. One 2008 meta-analysis examined genetic variants in 16 genes and found nominally significant effects.
Other research has suggested that a greater than average number of rare deletions or duplications of tiny DNA sequences within genes (known as copy number variants) are linked to increased risk for schizophrenia, especially in those “sporadic” cases not linked to family history of schizophrenia, and that the genetic factors and developmental pathways can thus be different in different individuals. A genome wide survey of 3,391 individuals with schizophrenia found CNVs in less than 1% of cases. Within them, deletions in regions related to psychosis were observed, as well as deletions on chromosome 15q13.3 and 1q21.1.
CNVs occur due to non-allelic homologous recombination mediated by low copy repeats (sequentially similar regions). This results in deletions and duplications of dosage sensitive genes. It has been speculated that CNVs underlie a significant proportion of normal human variation, including differences in cognitive, behavioral, and psychological features, and that CNVs in at least three loci can result in increased risk for schizophrenia in a few individuals. Epigenetics may also play a role in schizophrenia, with the expression of Protocadherin 11 X/Protocadherin Y playing a possible role in schizophrenia.
A 2009 study was able to create mice matching schizophrenic symptoms by the deletion of only one gene set, those of the neuregulin post-synaptic receptor. The result showed that although the mice mostly developed normally, on further brain development, glutamate receptors brokedown. This theory supports the glutamate hypothesis of schizophrenia. Another study in 2009 by Simon Fraser University researchers identifies a link between Autism and Schizophrenia :
“The SFU group found that variations in four sets of genes are related to both autism and schizophrenia. People normally have two copies of each gene, but in autistics some genome locations have only single copies and in schizophrenics extra copies are present at the same locations.” “Source”
Prenatal
It is well established that obstetric complications or events are associated with an increased chance of the child later developing schizophrenia, although overall they constitute a non-specific risk factor with a relatively small effect. Obstetric complications occur in approximately 25 to 30% of the general population and the vast majority do not develop schizophrenia, and likewise the majority of individuals with schizophrenia have not had a detectable obstetric event. Nevertheless, the increased average risk is well-replicated, and such events may moderate the effects of genetic or other environmental risk factors. The specific complications or events most linked to schizophrenia, and the mechanisms of their effects, are still under examination.
One epidemiological finding is that people diagnosed with schizophrenia are more likely to have been born in winter or spring (at least in the northern hemisphere). However, the effect is not large. Explanations have included a greater prevalence of viral infections at that time, or a greater likelihood of vitamin D deficiency. A similar effect (increased likelihood of being born in winter and spring) has also been found with other, healthy populations, such as chess players.
Women who were pregnant during the Dutch famine of 1944, where many people were close to starvation (experiencing malnutrition) had a higher chance of having a child who would later develop schizophrenia. Studies of Finnish mothers who were pregnant when they found out that their husbands had been killed during the Winter War of 1939–1940 have shown that their children were significantly more likely to develop schizophrenia when compared with mothers who found out about their husbands’ death after pregnancy, suggesting that maternal stress may have an effect.
Fetal growth
Lower than average birth weight has been one of the most consistent findings, indicating slowed fetal growth possibly mediated by genetic effects. Almost any factor adversely affecting the fetus will affect growth rate, however, so the association has been described as not particularly informative regarding causation. In addition, the majority of birth cohort studies have failed to find a link between schizophrenia and low birth weight or other signs of growth retardation.
Animal models have suggested links between intrauterine growth restriction and specific neurological abnormalities similar to those that may be involved in the development of schizophrenia, including ventricular enlargement and reduced hippocampal volume in guinea pigs.
Hypoxia
It has been hypothesized since the 1970s that brain hypoxia (low oxygen levels) before, at or immediately after birth may be a risk factor for the development of schizophrenia.
Hypoxia is now being demonstrated as relevant to schizophrenia in animal models, molecular biology and epidemiology studies. One study in Molecular Psychiatry was able to differentiate 90% of schizophrenics from controls based on hypoxia and metabolism. Hypoxia has been recently described as one of the most important of the external factors that influence susceptibility, although studies have been mainly epidemiological. Such studies place a high degree of importance on hypoxic influence, but because of familial pattern of the illness in some families, propose a genetic factor also; stopping short of concluding hypoxia to be the sole cause. Fetal hypoxia, in the presence of certain unidentified genes, has been correlated with reduced volume of the hippocampus, which is in turn correlated with schizophrenia.
Although most studies have interpreted hypoxia as causing some form of neuronal dysfunction or even subtle damage, it has been suggested that the physiological hypoxia that prevails in normal embryonic and fetal development, or pathological hypoxia or ischemia, may exert an effect by regulating or dysregulating genes involved in neurodevelopment. A literature review judged that over 50% of the candidate genes for susceptibility to schizophrenia met criteria for “ischemia–hypoxia regulation and/or vascular expression” even though only 3.5% of all genes were estimated to be involved in hypoxia/ischemia or the vasculature.
A longitudinal study found that obstetric complications involving hypoxia were one factor associated with neurodevelopmental impairments in childhood and with the later development of schizophreniform disorders. Fetal hypoxia has been found to predict unusual movements at age 4 (but not age 7) among children who go on to develop schizophrenia, suggesting that its effects are specific to the stage of neurodevelopment. A Japanese case study of monozygotic twins discordant for schizophrenia (one has the diagnosis while the other does not) draws attention to their different weights at birth and concludes hypoxia may be the differentiating factor.
The unusual functional laterality in speech production (e.g. right hemisphere auditory processing) found in some individuals with schizophrenia could be due to aberrant neural networks established as a compensation for left temporal lobe damage induced by pre- or perinatal hypoxia. Prenatal and perinatal hypoxia appears to be important as one factor in the neurodevelopmental model, with the important implication that some forms of schizophrenia may thus be preventable.
Research on rodents seeking to understand the possible role of prenatal hypoxia in disorders such as schizophrenia has indicated that it can lead to a range of sensorimotor and learning/memory abnormalities. Impairments in motor function and coordination, evident on challenging tasks when the hypoxia was severe enough to cause brain damage, were long-lasting and described as a “hallmark of prenatal hypoxia”.
Several animal studies have indicated that fetal hypoxia can affect many of the same neural substrates implicated in schizophrenia, depending on the severity and duration of the hypoxic event as well as the period of gestation, and in humans moderate or severe (but not mild) fetal hypoxia has been linked to a series of motor, language and cognitive deficits in children, regardless of genetic liability to schizophrenia. One paper restated that cerebellum neurological disorders were frequently found in schizophrenics and speculated hypoxia may cause the subsequent cognitive dysmetria
Whereas most studies find only a modest effect of hypoxia in schizophrenia, a longitudinal study using a combination of indicators to detect possible fetal hypoxia, such as early equivalents of Neurological Soft Signs or obstetric complications, reported that the risk of schizophrenia and other nonaffective psychoses was “strikingly elevated” (5.75% versus 0.39%). Although objective estimates of hypoxia did not account for all schizophrenic cases; the study revealed increasing odds of schizophrenia according to graded increase in severity of hypoxia.
Other factors
There is an emerging literature on a wide range of prenatal risk factors, such as prenatal stress, intrauterine (in the womb) malnutrition, and prenatal infection. Increased paternal age has been linked to schizophrenia, possibly due to “chromosomal aberrations and mutations of the aging germline.” Maternal-fetal rhesus or genotype incompatibility has also been linked, via increasing the risk of an adverse prenatal environment. Also, in mothers with schizophrenia, an increased risk has been identified via a complex interaction between maternal genotype, maternal behavior, prenatal environment and possibly medication and socioeconomic factors. References for many of these environmental risk factors have been collected in an online database.
There may be an association between celiac disease (gluten intolerance) and schizophrenia in a small proportion of patients, though large randomized controlled trials and epidemiological studies will be needed before such an association can be confirmed. Withdrawal of gluten from the diet is an inexpensive measure which may improve the symptoms in a small (≤3%) number of schizophrenic patients.
In addition, there is some evidence that exposure to toxins such as lead can also increase the risk of later development of schizophrenia spectrum disorders.
Infections
Numerous viral infections, in utero or in childhood, have been associated with an increased risk of later developing schizophrenia. Schizophrenia is somewhat more common in those born in winter to early spring, when infections are more common.
Influenza has long been studied as a possible factor. A 1988 study found that individuals who were exposed to the Asian flu as second trimester fetuses were at increased risk of eventually developing schizophrenia. This result was corroborated by a later British study of the same pandemic, but not by a 1994 study of the pandemic in Croatia. A Japanese study also found no support for a link between schizophrenia and birth after an influenza epidemic.
Polio, measles, varicella-zoster, rubella, herpes simplex virus type 2, maternal genital infections, Borna disease virus, and more recently Toxoplasma gondii, have been correlated with the later development of schizophrenia. Psychiatrists E. Fuller Torrey and R.H. Yolken have hypothesized that the latter, a common parasite in humans, contributes to some, if not many, cases of schizophrenia.
In a meta-analysis of several studies, they found moderately higher levels of Toxoplasma antibodies in those with schizophrenia and possibly higher rates of prenatal or early postnatal exposure to Toxoplasma gondii, but not acute infection. However, in another study of postmortem brain tissue, the authors have reported equivocal or negative results, including no evidence of herpes virus or T. gondii involvement in schizophrenia.
There is some evidence for the role of autoimmunity in the development of some cases of schizophrenia. A statistical correlation has been reported with various autoimmune diseases and direct studies have linked dysfunctional immune status to some of the clinical features of schizophrenia.
This is known as the pathogenic theory of schizophrenia or germ theory of schizophrenia. It is a pathogenic theory of disease in which it is thought that a proximal cause of certain cases of schizophrenia is the interaction of the developing fetus with pathogens such as viruses, or with antibodies from the mother created in response to these pathogens (in particular, Interleukin 8). Substantial research suggests that exposure to certain illnesses (e.g., influenza) in the mother of the neonate (especially at the end of the second trimester) causes defects in neural development which may emerge as a predisposition to schizophrenia around the time of puberty, as the brain grows and develops.
Childhood antecedents
In general, the antecedents of schizophrenia are subtle and those who will go on to develop schizophrenia do not form a readily identifiable subgroup – which would lead to identification of a specific cause. Average group differences from the norm may be in the direction of superior as well as inferior performance. Overall, birth cohort studies have indicated subtle nonspecific behavioral features, some evidence for psychotic-like experiences (particularly hallucinations), and various cognitive antecedents. There have been some inconsistencies in the particular domains of functioning identified and whether they continue through childhood and whether they are specific to schizophrenia.
A prospective study found average differences across a range of developmental domains, including reaching milestones of motor development at a later age, having more speech problems, lower educational test results, solitary play preferences at ages four and six, and being more socially anxious at age 13. Lower ratings of the mother’s skills and understanding of the child at age 4 were also related.
Some of the early developmental differences were identified in the first year of life in a study in Finland, although generally related to psychotic disorders rather than schizophrenia in particular. The early subtle motor signs persisted to some extent, showing a small link to later school performance in adolescence. An earlier Finnish study found that childhood performance of 400 individuals diagnosed with schizophrenia was significantly worse than controls on subjects involving motor co-ordination (sports and handcrafts) between ages 7 and 9, but there were no differences on academic subjects (contrary to some other IQ findings). (Patients in this age group with these symptoms were significantly less likely to progress to high school, despite academic ability)
However, reanalysis of the data from the later Finnish study, on older children (14 to 16) in a changed school system, using narrower diagnostic criteria and with less cases but more controls, did not support a significant difference on sports and handicraft performance. However, another study found that unusual motor coordination scores at 7 years of age were associated in adulthood with both those with schizophrenia and their unaffected siblings, while unusual movements at ages 4 and 7 predicted adult schizophrenia but not unaffected sibling status.
A birth cohort study in New Zealand found that children who went on to develop schizophreniform disorder had, as well as emotional problems and interpersonal difficulties linked to all adult psychiatric outcomes measured, significant impairments in neuromotor, receptive language, and cognitive development. A retrospective study found that adults with schizophrenia had performed better than average in artistic subjects at ages 12 and 15, and in linguistic and religious subjects at age 12, but worse than average in gymnastics at age 15.
Some small studies on offspring of individuals with schizophrenia have identified various neurobehavioral deficits, a poorer family environment and disruptive school behaviour, poor peer engagement, immaturity or unpopularity or poorer social competence and increasing schizophrenic symptomology emerging during adolescence.
A minority “deficit syndrome” subtype of schizophrenia is proposed to be more marked by early poor adjustment and behavioral problems, as compared to non-deficit subtypes.
Substance use
The relationship between schizophrenia and drug use is complex, meaning that a clear causal connection between drug use and schizophrenia has been difficult to tease apart. There is strong evidence that using certain drugs can trigger either the onset or relapse of schizophrenia in some people. It may also be the case, however, that people with schizophrenia use drugs to overcome negative feelings associated with both the commonly prescribed antipsychotic medication and the condition itself, where negative emotion, paranoia and anhedonia are all considered to be core features.
The rate of substance use is known to be particularly high in this group. In a recent study, 60% of people with schizophrenia were found to use substances and 37% would be diagnosable with a substance use disorder.
Cannabis
There is some evidence that cannabis use can contribute to schizophrenia. Some studies suggest that cannabis is neither a sufficient nor necessary factor in developing schizophrenia, but that cannabis may significantly increase the risk of developing schizophrenia and may be, among other things, a significant causal factor. Nevertheless, some previous research in this area has been criticised as it has often not been clear whether cannabis use is a cause or effect of schizophrenia. To address this issue, a recent review of studies from which a causal contribution to schizophrenia can be assessed has suggested that cannabis statistically doubles the risk of developing schizophrenia on the individual level, and may, assuming a causal relationship, be responsible for up to 8% of cases in the population.
An older longitudinal study, published in 1987, suggested a sixfold increase of schizophrenia risks for high consumers of cannabis (use on more than fifty occasions) in Sweden.
Despite increases in cannabis consumption in the 1960s and 1970s in western society, rates of psychotic disorders such as schizophrenia remained relatively stable over time. Also, Sweden and Japan, where self-reported marijuana use is very low, do not have lower rates of psychosis than the U.S. and Canada do. Thus, there remains controversy over whether or not the apparent association between cannabis and schizophrenia is a causal relationship.
Amphetamines and other stimulants
As amphetamines trigger the release of dopamine and excessive dopamine function is believed to be responsible for many symptoms of schizophrenia (known as the dopamine hypothesis of schizophrenia), amphetamines may worsen schizophrenia symptoms. In addition, amphetamines are known to cause a stimulant psychosis in otherwise healthy individuals that superficially resembles schizophrenia, and may be misdiagnosed as such by some healthcare professionals.
Hallucinogens
Drugs such as ketamine, PCP, and LSD have been used to mimic schizophrenia for research purposes. Using LSD and other psychedelics as a model has now fallen out of favor with the scientific research community, as the differences between the drug induced states and the typical presentation of schizophrenia have become clear. The dissociatives ketamine and PCP, however, are still considered to produce states that are remarkably similar however, and are considered to be even better models than stimulants since they produce both positive and negative symptoms.
Tobacco use
People with schizophrenia tend to smoke significantly more tobacco than the general population. The rates are exceptionally high amongst institutionalized patients and homeless people. In a UK census from 1993, 74% of people with schizophrenia living in institutions were found to be smokers. A 1999 study that covered all people with schizophrenia in Nithsdale, Scotland found a 58% prevalence rate of cigarette smoking, to compare with 28% in the general population. An older study found that as much as 88% of outpatients with schizophrenia were smokers.
Despite the higher prevalence of tobacco smoking, people diagnosed with schizophrenia have a much lower than average chance of developing and dying from lung cancer. While the reason for this is unknown, it may be because of a genetic resistance to the cancer, a side effect of drugs being taken, or a statistical effect of increased likelihood of dying from causes other than lung cancer.
A 2003 study of over 50,000 Swedish conscripts found that there was a small but significant protective effect of smoking cigarettes on the risk of developing schizophrenia later in life. While the authors of the study stressed that the risks of smoking far outweigh these minor benefits, this study provides further evidence for the ‘self-medication’ theory of smoking in schizophrenia and may give clues as to how schizophrenia might develop at the molecular level. Furthermore, many people with schizophrenia have smoked tobacco products long before they are diagnosed with the illness, and a cohort study of Israeli conscripts found that healthy adolescent smokers were more likely to develop schizophrenia in the future than their nonsmoking peers.
It is of interest that cigarette smoking affects liver function such that the antipsychotic drugs used to treat schizophrenia are broken down in the blood stream more quickly. This means that smokers with schizophrenia need slightly higher doses of antipsychotic drugs in order for them to be effective than do their non-smoking counterparts.
The increased rate of smoking in schizophrenia may be due to a desire to self-medicate with nicotine. One possible reason is that smoking produces a short term effect to improve alertness and cognitive functioning in persons who suffer this illness. It has been postulated that the mechanism of this effect is that people with schizophrenia have a disturbance of nicotinic receptor functioning which is temporarily abated by tobacco use. However, some researchers have questioned whether self-medication is really the best explanation for the association.
A study from 1989 and a 2004 case study show that when haloperidol is administered, nicotine limits the extent to which the antipsychotic increases the sensitivity of the dopamine 2 receptor. Dependent on the dopamine system, symptoms of Tardive Dyskinesia are not found in the nicotine administered patients despite a roughly 70% increase in dopamine receptor activity, but the controls have more than 90% and do develop symptoms.A 1997 study showed that akathisia was significantly reduced upon administration of nicotine when the akathisia was induced by antipsychotics. This gives credence to the idea tobacco could be used to self medicate by limiting effects of the illness, the medication, or both.
Life experiences
Social adversity
The chance of developing schizophrenia has been found to increase with the number of adverse social factors (e.g. indicators of socioeconomic disadvantage or social exclusion) present in childhood. Stressful life events generally precede the onset of schizophrenia. A personal or recent family history of migration is a considerable risk factor for schizophrenia, which has been linked to psychosocial adversity, social defeat from being an outsider, racial discrimination, family dysfunction, unemployment and poor housing conditions.
Childhood experiences of abuse or trauma are risk factors for a diagnosis of schizophrenia later in life. Recent large-scale general population studies indicate the relationship is a causal one, with an increasing risk with additional experiences of maltreatment, although a critical review suggests conceptual and methodological issues require further research. There is some evidence that adversities may lead to cognitive biases and/or altered dopamine neurotransmission, a process that has been termed “sensitization”.
Specific social experiences have been linked to specific psychological mechanisms and psychotic experiences in schizophrenia. In addition, structural neuroimaging studies of victims of sexual abuse and other traumas have sometimes reported findings similar to those sometimes found in psychotic patients, such as thinning of the corpus callosum, loss of volume in the anterior cingulate cortex, and reduced hippocampal volume.
Urbanicity
A particularly stable and replicable finding has been the association between living in an urban environment and the development of schizophrenia, even after factors such as drug use, ethnic group and size of social group have been controlled for. A recent study of 4.4 million men and women in Sweden found a 68%–77% increased risk of diagnosed psychosis for people living in the most urbanized environments, a significant proportion of which is likely to be described as schizophrenia.
The effect does not appear to be due to a higher incidence of obstetric complications in urban environments. The risk increases with the number of years and degree of urban living in childhood and adolescence, suggesting that constant, cumulative, or repeated exposures during upbringing occurring more frequently in urbanized areas are responsible for the association.
Various possible explanations for the effect have been judged unlikely based on the nature of the findings, including infectious causes or a generic stress effect. It is thought to interact with genetic dispositions and, since there appears to be nonrandom variation even across different neighborhoods, and an independent association with social isolation, it has been proposed that the degree of “social capital” (e.g. degree of mutual trust, bonding and safety in neighborhoods) can exert a developmental impact on children growing up in these environments.
Close relationships
Evidence is consistent that negative attitudes from others increase the risk of schizophrenia relapse, in particular critical comments, hostility, authoritarian, and intrusive or controlling attitudes (termed ‘high expressed emotion’ by researchers). Although family members and significant others are not held responsible for schizophrenia – the attitudes, behaviors and interactions of all parties are addressed – unsupportive dysfunctional relationships may also contribute to an increased risk of developing schizophrenia.
Other proposed etiologies
Psychiatrists R. D. Laing, Silvano Arieti, Theodore Lidz and others have argued that the symptoms of what is called mental illness are comprehensible reactions to impossible demands that society and particularly family life places on some sensitive individuals. Laing, Arieti and Lidz were notable in valuing the content of psychotic experience as worthy of interpretation, rather than considering it simply as a secondary and essentially meaningless marker of underlying psychological or neurological distress. Laing described eleven case studies of people diagnosed with schizophrenia and argued that the content of their actions and statements was meaningful and logical in the context of their family and life situations.
In 1956, Gregory Bateson and his colleagues Paul Watzlawick, Donald Jackson, and Jay Haley articulated a theory of schizophrenia, related to Laing’s work, as stemming from double bind situations where a person receives different or contradictory messages. Madness was therefore an expression of this distress and should be valued as a cathartic and transformative experience. In the books Schizophrenia and the Family and The Origin and Treatment of Schizophrenic Disorders Lidz and his colleagues explain their belief that parental behaviour can result in mental illness in children. Arieti’s Interpretation of Schizophrenia won the 1975 scientific National Book Award in the United States.
The concept of schizophrenia as a result of civilization has been developed further by psychologist Julian Jaynes in his 1976 book The Origin of Consciousness in the Breakdown of the Bicameral Mind; he proposed that until the beginning of historic times, schizophrenia or a similar condition was the normal state of human consciousness. This would take the form of a “bicameral mind” where a normal state of low affect, suitable for routine activities, would be interrupted in moments of crisis by “mysterious voices” giving instructions, which early people characterized as interventions from the gods. Researchers into shamanism have speculated that in some cultures schizophrenia or related conditions may predispose an individual to becoming a shaman; the experience of having access to multiple realities is not uncommon in schizophrenia, and is a core experience in many shamanic traditions. Equally, the shaman may have the skill to bring on and direct some of the altered states of consciousness psychiatrists label as illness. Psychohistorians, on the other hand, accept the psychiatric diagnoses. However, unlike the current medical model of mental disorders they may argue that poor parenting in tribal societies causes the shaman’s schizoid personalities. Commentators such as Paul Kurtz and others have endorsed the idea that major religious figures experienced psychosis, heard voices and displayed delusions of grandeur.
Modern clinical psychological research has indicated a number of processes which may cause or bring on episodes of schizophrenia.
A number of cognitive biases and deficits have been identified. These include attribution biases in social situations, difficulty distinguishing inner speech from speech from an external source (source monitoring), difficulty in adjusting speech to the needs of the hearer, difficulties in the very earliest stages of processing visual information (including reduced latent inhibition), and an attentional bias towards threats.
Some of these tendencies have been shown to worsen or appear when under emotional stress or in confusing situations. As with related neurological findings, they are not shown by all individuals with a diagnosis of schizophrenia, and it is not clear how specific they are to schizophrenia. However, the findings regarding cognitive difficulties in schizophrenia are reliable and consistent enough for some researchers to argue that they are diagnostic.
Impaired capacity to appreciate one’s own and others’ mental states has been reported to be the single-best predictor of poor social competence in schizophrenia, and similar cognitive features have been identified in close relatives of people diagnosed with schizophrenia.
A number of emotional factors have been implicated in schizophrenia, with some models putting them at the core of the disorder. It was thought that the appearance of blunted affect meant that sufferers did not experience strong emotions, but more recent studies indicate there is often a normal or even heightened level of emotionality, particularly in response to negative events or stressful social situations. Some theories suggest positive symptoms of schizophrenia can result from or be worsened by negative emotions, including depressed feelings and low self-esteem and feelings of vulnerability, inferiority or loneliness. Chronic negative feelings and maladaptive coping skills may explain some of the association between psychosocial stressors and symptomology. Critical and controlling behaviour by significant others (high expressed emotion) causes increased emotional arousal and lowered self-esteem and a subsequent increase in positive symptoms such as unusual thoughts. Countries or cultures where schizotypal personalities or schizophrenia symptoms are more accepted or valued appear to be associated with reduced onset of, or increased recovery from, schizophrenia.
Related studies suggest that the content of delusional and psychotic beliefs in schizophrenia can be meaningful and play a causal or mediating role in reflecting the life history, or social circumstances of the individual. Holding minority socio-cultural beliefs, for example due to ethnic background, has been linked to increased diagnosis of schizophrenia. The way an individual interprets his or her delusions and hallucinations (e.g. as threatening or as potentially positive) has also been found to influence functioning and recovery.
Some experts think autonomy vs intimacy is a motivation for schizophrenic symptoms.
Other lines of work relating to the self in schizophrenia have linked it to psychological dissociation or abnormal states of awareness and identity as understood from phenomenological and other perspectives.
Psychiatrist Tim Crow has argued that schizophrenia may be the evolutionary price we pay for a left brain hemisphere specialization for language. Since psychosis is associated with greater levels of right brain hemisphere activation and a reduction in the usual left brain hemisphere dominance, our language abilities may have evolved at the cost of causing schizophrenia when this system breaks down.
In alternative medicine, some practitioners believe that there are a vast number of physical causes of what ends up being diagnosed as schizophrenia. While some of these explanations may stretch credulity, others (such as heavy metal poisoning and nutritional imbalances) have been supported at least somewhat by research. However, it is not entirely clear how many patients initially diagnosed with schizophrenia these alternative explanations may account for.
Mechanisms
A number of attempts have been made to explain the link between altered brain function and schizophrenia. One of the most common is the dopamine hypothesis, which attributes psychosis to the mind’s faulty interpretation of the misfiring of dopaminergic neurons.
Psychological
Many psychological mechanisms have been implicated in the development and maintenance of schizophrenia. Cognitive biases have been identified in those with the diagnosis or those at risk, especially when under stress or in confusing situations. Some cognitive features may reflect global neurocognitive deficits such as memory loss, while others may be related to particular issues and experiences.
Despite a demonstrated appearance of “blunted affect”, recent findings indicate that many individuals diagnosed with schizophrenia are emotionally responsive, particularly to stressful or negative stimuli, and that such sensitivity may cause vulnerability to symptoms or to the disorder. Some evidence suggests that the content of delusional beliefs and psychotic experiences can reflect emotional causes of the disorder, and that how a person interprets such experiences can influence symptomatology. The use of “safety behaviors” to avoid imagined threats may contribute to the chronicity of delusions. Further evidence for the role of psychological mechanisms comes from the effects of psychotherapies on symptoms of schizophrenia.
Neurological
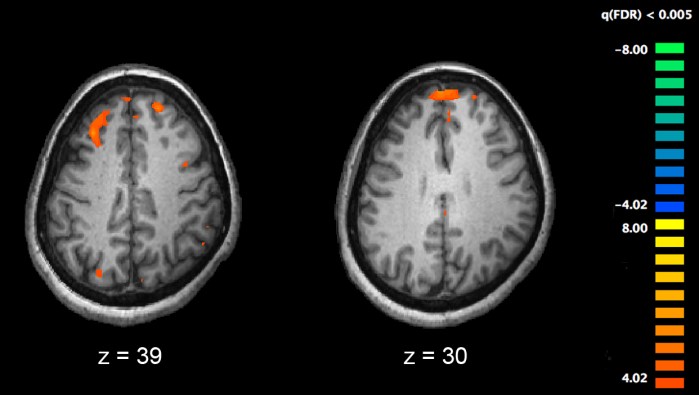
Functional magnetic resonance imaging (fMRI), and other brain imaging technologies, allow for the study of differences in brain activity in people diagnosed with schizophrenia. The image shows two levels of the brain, with areas that were more active in healthy controls than in schizophrenia patients shown in red, during an fMRI study of working memory.
Those with a diagnosis of schizophrenia have changes in both brain structure and chemistry. Studies using neuropsychological tests and brain imaging technologies such as fMRI and PET to examine functional differences in brain activity have shown that differences seem to most commonly occur in the frontal lobes, hippocampus and temporal lobes. Reductions in brain volume, smaller than those found in Alzheimer’s disease, have been reported in areas of the frontal cortex and temporal lobes. It is uncertain whether these volumetric changes are progressive or preexist prior to the onset of the disease. These differences have been linked to the neurocognitive deficits often associated with schizophrenia. Because neural circuits are altered, it has alternatively been suggested that schizophrenia should be thought of as a collection of neurodevelopmental disorders.
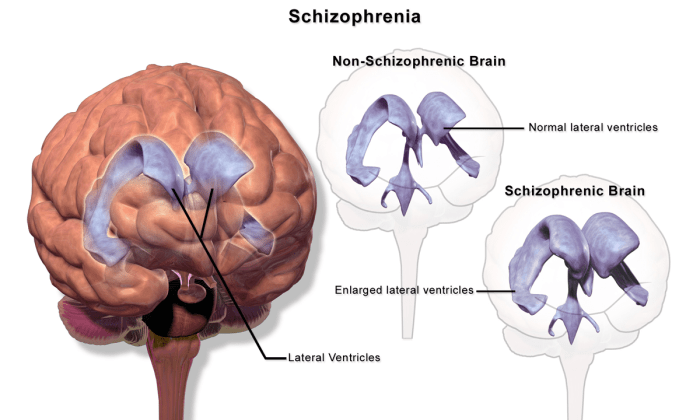
People with schizophrenia who are medication compliant have an association with enlarged lateral ventricles in the brain.
Particular attention has been paid to the function of dopamine in the mesolimbic pathway of the brain. This focus largely resulted from the accidental finding that phenothiazine drugs, which block dopamine function, could reduce psychotic symptoms. It is also supported by the fact that amphetamines, which trigger the release of dopamine, may exacerbate the psychotic symptoms in schizophrenia. The influential dopamine hypothesis of schizophrenia proposed that excessive activation of D2 receptors was the cause of (the positive symptoms of) schizophrenia. Although postulated for about 20 years based on the D2 blockade effect common to all antipsychotics, it was not until the mid-1990s that PET and SPET imaging studies provided supporting evidence. The dopamine hypothesis is now thought to be simplistic, partly because newer antipsychotic medication (atypical antipsychotic medication) can be just as effective as older medication (typical antipsychotic medication), but also affects serotonin function and may have slightly less of a dopamine blocking effect.
Interest has also focused on the neurotransmitter glutamate and the reduced function of the NMDA glutamate receptor in schizophrenia, largely because of the abnormally low levels of glutamate receptors found in the postmortem brains of those diagnosed with schizophrenia, and the discovery that glutamate-blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with the condition. Reduced glutamate function is linked to poor performance on tests requiring frontal lobe and hippocampal function, and glutamate can affect dopamine function, both of which have been implicated in schizophrenia, have suggested an important mediating (and possibly causal) role of glutamate pathways in the condition. But positive symptoms fail to respond to glutamatergic medication.
Diagnosis
Schizophrenia is diagnosed based on criteria in either the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, version DSM-IV-TR, or the World Health Organization’s International Statistical Classification of Diseases and Related Health Problems, the ICD-10. These criteria use the self-reported experiences of the person and reported abnormalities in behavior, followed by a clinical assessment by a mental health professional. Symptoms associated with schizophrenia occur along a continuum in the population and must reach a certain severity before a diagnosis is made. As of 2009 there is no objective test.
John Nash, a U.S. mathematician and joint winner of the 1994 Nobel Prize for Economics, suffered from schizophrenia. His life has been the subject of the 2001 Academy Award-winning film A Beautiful Mind.
Criteria
The ICD-10 criteria are typically used in European countries, while the DSM-IV-TR criteria are used in the United States and the rest of the world, and are prevailing in research studies. The ICD-10 criteria put more emphasis on Schneiderian first-rank symptoms. In practice, agreement between the two systems is high.
According to the revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), to be diagnosed with schizophrenia, three diagnostic criteria must be met:
Characteristic symptoms: Two or more of the following, each present for much of the time during a one-month period (or less, if symptoms remitted with treatment).
- Delusions
- Hallucinations
- Disorganized speech, which is a manifestation of formal thought disorder
- Grossly disorganized behavior (e.g. dressing inappropriately, crying frequently) or catatonic behavior
- Negative symptoms: Blunted affect (lack or decline in emotional response), alogia (lack or decline in speech), or avolition (lack or decline in motivation)
If the delusions are judged to be bizarre, or hallucinations consist of hearing one voice participating in a running commentary of the patient’s actions or of hearing two or more voices conversing with each other, only that symptom is required above. The speech disorganization criterion is only met if it is severe enough to substantially impair communication.
- Social or occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset.
- Significant duration: Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms (or less, if symptoms remitted with treatment).
If signs of disturbance are present for more than a month but less than six months, the diagnosis of schizophreniform disorder is applied. Psychotic symptoms lasting less than a month may be diagnosed as brief psychotic disorder, and various conditions may be classed as psychotic disorder not otherwise specified. Schizophrenia cannot be diagnosed if symptoms of mood disorder are substantially present (although schizoaffective disorder could be diagnosed), or if symptoms of pervasive developmental disorder are present unless prominent delusions or hallucinations are also present, or if the symptoms are the direct physiological result of a general medical condition or a substance, such as abuse of a drug or medication.
Subtypes
The DSM-IV-TR contains five sub-classifications of schizophrenia, although the developers of DSM-5 are recommending they be dropped from the new classification:
- Paranoid type: Where delusions and hallucinations are present but thought disorder, disorganized behavior, and affective flattening are absent. (DSM code 295.3/ICD code F20.0)
- Disorganized type: Named hebephrenic schizophrenia in the ICD. Where thought disorder and flat affect are present together. (DSM code 295.1/ICD code F20.1)
- Catatonic type: The subject may be almost immobile or exhibit agitated, purposeless movement. Symptoms can include catatonic stupor and waxy flexibility. (DSM code 295.2/ICD code F20.2)
- Undifferentiated type: Psychotic symptoms are present but the criteria for paranoid, disorganized, or catatonic types have not been met. (DSM code 295.9/ICD code F20.3)
- Residual type: Where positive symptoms are present at a low intensity only. (DSM code 295.6/ICD code F20.5)
The ICD-10 defines two additional subtypes:
- Post-schizophrenic depression: A depressive episode arising in the aftermath of a schizophrenic illness where some low-level schizophrenic symptoms may still be present. (ICD code F20.4)
- Simple schizophrenia: Insidious and progressive development of prominent negative symptoms with no history of psychotic episodes. (ICD code F20.6)
Differential
Psychotic symptoms may be present in several other mental disorders, including bipolar disorder, borderline personality disorder, drug intoxication and drug-induced psychosis. Delusions (“non-bizarre”) are also present in delusional disorder, and social withdrawal in social anxiety disorder, avoidant personality disorder and schizotypal personality disorder. Schizophrenia is complicated with obsessive-compulsive disorder (OCD) considerably more often than could be explained by pure chance, although it can be difficult to distinguish obsessions that occur in OCD from the delusions of schizophrenia.
A more general medical and neurological examination may be needed to rule out medical illnesses which may rarely produce psychotic schizophrenia-like symptoms, such as metabolic disturbance, systemic infection, syphilis, HIV infection, epilepsy, and brain lesions. It may be necessary to rule out a delirium, which can be distinguished by visual hallucinations, acute onset and fluctuating level of consciousness, and indicates an underlying medical illness. Investigations are not generally repeated for relapse unless there is a specific medical indication or possible adverse effects from antipsychotic medication.
Prevention
Evidence for the effectiveness of early intervention is inconclusive. While there is some evidence that early intervention in those with a psychotic episode may improve short term outcomes, there is little benefit from these measures after five years. Attempting to prevent schizophrenia in the prodrome phase is of uncertain benefit and therefore as of 2009 is not recommended. Prevention is difficult as there are no reliable markers for the later development of the disease.
Management
The primary treatment of schizophrenia is antipsychotic medications, often in combination with psychological and social supports. Hospitalization may occur for severe episodes either voluntarily or (if mental health legislation allows it) involuntarily. Long-term hospitalization is uncommon since deinstitutionalization beginning in the 1950s, although still occurs. Community support services including drop-in centers, visits by members of a community mental health team, supported employment and support groups are common. Some evidence indicates that regular exercise has a positive effect on the physical and mental health of those with schizophrenia.
Medication

Risperidone (trade name Risperdal) is a common atypical antipsychotic medication.
The first-line psychiatric treatment for schizophrenia is antipsychotic medication, which can reduce the positive symptoms of psychosis in about 7–14 days. Antipsychotics however fail to significantly ameliorate the negative symptoms and cognitive dysfunction.
The choice of which antipsychotic to use is based on benefits, risks, and costs. It is debatable whether, as a class, typical or atypical antipsychotics are better. Both have equal drop-out and symptom relapse rates when typicals are used at low to moderate dosages. There is a good response in 40–50%, a partial response in 30–40%, and treatment resistance (failure of symptoms to respond satisfactorily after six weeks to two of three different antipsychotics) in 20% of people. Clozapine is an effective treatment for those who respond poorly to other drugs, but it has the potentially serious side effect of agranulocytosis (lowered white blood cell count) in 1–4%.
With respect to side effects typical antipsychotics are associated with a higher rate of extrapyramidal side effects while atypicals are associated with considerable weight gain, diabetes and risk of metabolic syndrome. While atypicals have fewer extrapyramidal side effects these differences are modest. Some atypicals such as quetiapine and risperidone are associated with a higher risk of death compared to the atypical perphenazine, while clozapine is associated with the lowest risk of death. It remains unclear whether the newer antipsychotics reduce the chances of developing neuroleptic malignant syndrome, a rare but serious neurological disorder.
For people who are unwilling or unable to take medication regularly, long-acting depot preparations of antipsychotics may be used to achieve control. When used in combination with psychosocial interventions they may improve long-term adherence to treatment.
Psychosocial
A number of psychosocial interventions may be useful in the treatment of schizophrenia including: family therapy, assertive community treatment, supported employment, cognitive remediation, skills training, cognitive behavioral therapy (CBT), token economic interventions, and psychosocial interventions for substance use and weight management. Family therapy or education, which addresses the whole family system of an individual, may reduce relapses and hospitalizations. The evidence for CBT’s effectiveness in either reducing symptoms or preventing relapse is minimal. The benefits of art or drama therapy are currently unknown.
Prognosis
Schizophrenia has great human and economic costs. It results in a decreased life expectancy of 12–15 years, primarily because of its association with obesity, sedentary lifestyles, and smoking, with an increased rate of suicide playing a lesser role. These differences in life expectancy increased between the 1970s and 1990s, and between the 1990s and first decade of the 21st century did not change substantially in a health system with open access to care (Finland).
Schizophrenia is a major cause of disability, with active psychosis ranked as the third-most-disabling condition after quadriplegia and dementia and ahead of paraplegia and blindness. Approximately three-fourths of people with schizophrenia have ongoing disability with relapses. Some people do recover completely and others function well in society. Most people with schizophrenia live independently with community support. In people with a first episode of psychosis a good long-term outcome occurs in 42%, an intermediate outcome in 35% and a poor outcome in 27%. Outcomes for schizophrenia appear better in the developing than the developed world. These conclusions however have been questioned.
There is a higher than average suicide rate associated with schizophrenia. This has been cited at 10%, but a more recent analysis of studies and statistics revises the estimate to 4.9%, most often occurring in the period following onset or first hospital admission. Several times more (20 to 40%) attempt suicide at least once. There are a variety of risk factors, including male gender, depression, and a high intelligence quotient.
Schizophrenia and smoking have shown a strong association in studies world-wide. Use of cigarettes is especially high in individuals diagnosed with schizophrenia, with estimates ranging from 80% to 90% being regular smokers, as compared to 20% of the general population. Those who smoke tend to smoke heavily, and additionally smoke cigarettes with high nicotine content.
Epidemiology
Schizophrenia affects around 0.3–0.7% of people at some point in their life, or 24 million people worldwide as of 2011. It occurs 1.4 times more frequently in males than females and typically appears earlier in men—the peak ages of onset are 20–28 years for males and 26–32 years for females. Onset in childhood is much rarer, as is onset in middle- or old age. Despite the received wisdom that schizophrenia occurs at similar rates worldwide, its prevalence varies across the world, within countries, and at the local and neighborhood level. It causes approximately 1% of worldwide disability adjusted life years. The rate of schizophrenia varies up to threefold depending on how it is defined.
History
Accounts of a schizophrenia-like syndrome are thought to be rare in the historical record before the 19th century, although reports of irrational, unintelligible, or uncontrolled behavior were common. A detailed case report in 1797 concerning James Tilly Matthews, and accounts by Phillipe Pinel published in 1809, are often regarded as the earliest cases of the illness in the medical and psychiatric literature. Schizophrenia was first described as a distinct syndrome affecting teenagers and young adults by Bénédict Morel in 1853, termed démence précoce (literally ‘early dementia’). The term dementia praecox was used in 1891 by Arnold Pick in a case report of a psychotic disorder. In 1893 Emil Kraepelin introduced a broad new distinction in the classification of mental disorders between dementia praecox and mood disorder (termed manic depression and including both unipolar and bipolar depression). Kraepelin believed that dementia praecox was primarily a disease of the brain, and particularly a form of dementia, distinguished from other forms of dementia such as Alzheimer’s disease which typically occur later in life.
The word schizophrenia—which translates roughly as “splitting of the mind” and comes from the Greek roots schizein (σχίζειν, “to split”) and phrēn, phren- (φρήν, φρεν-, “mind”)—was coined by Eugen Bleuler in 1908 and was intended to describe the separation of function between personality, thinking, memory, and perception. Bleuler described the main symptoms as 4 A’s: flattened Affect, Autism, impaired Association of ideas and Ambivalence. Bleuler realized that the illness was not a dementia, as some of his patients improved rather than deteriorated, and thus proposed the term schizophrenia instead. Treatment was revolutionized in the mid-1950s with the development and introduction of chlorpromazine.
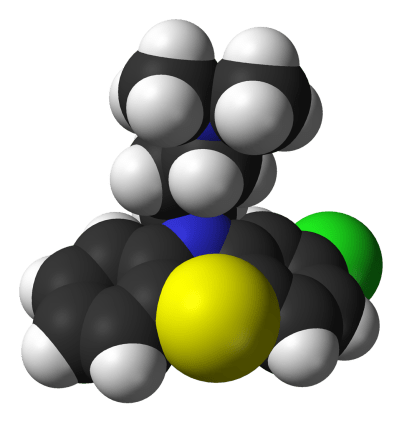
Molecule of chlorpromazine (trade name Thorazine), which revolutionized treatment of schizophrenia in the 1950s
In the early 1970s, the diagnostic criteria for schizophrenia was the subject of a number of controversies which eventually led to the operational criteria used today. It became clear after the 1971 US-UK Diagnostic Study that schizophrenia was diagnosed to a far greater extent in America than in Europe. This was partly due to looser diagnostic criteria in the US, which used the DSM-II manual, contrasting with Europe and its ICD-9. David Rosenhan’s 1972 study, published in the journal Science under the title “On being sane in insane places”, concluded that the diagnosis of schizophrenia in the US was often subjective and unreliable. These were some of the factors leading to the revision not only of the diagnosis of schizophrenia, but the revision of the whole DSM manual, resulting in the publication of the DSM-III in 1980.
The term schizophrenia is commonly misunderstood to mean that affected persons have a “split personality”. Although some people diagnosed with schizophrenia may hear voices and may experience the voices as distinct personalities, schizophrenia does not involve a person changing among distinct multiple personalities. The confusion arises in part due to the literal interpretation of Bleuler’s term schizophrenia. The first known misuse of the term to mean “split personality” was in an article by the poet T. S. Eliot in 1933.
Society and culture
Social stigma has been identified as a major obstacle in the recovery of patients with schizophrenia. In a large, representative sample from a 1999 study, 12.8% of Americans believed that individuals with schizophrenia were “very likely” to do something violent against others, and 48.1% said that they were “somewhat likely” to. Over 74% said that people with schizophrenia were either “not very able” or “not able at all” to make decisions concerning their treatment, and 70.2% said the same of money management decisions. The perception of individuals with psychosis as violent has more than doubled in prevalence since the 1950s, according to one meta-analysis.
In 2002 the term for schizophrenia in Japan was changed from Seishin-Bunretsu-Byō (mind-split-disease) to Tōgō-shitchō-shō (integration disorder) to reduce stigma. The new name was inspired by the biopsychosocial model; it increased the percentage of patients who were informed of the diagnosis from 37% to 70% over three years.
In the United States, the cost of schizophrenia—including direct costs (outpatient, inpatient, drugs, and long-term care) and non-health care costs (law enforcement, reduced workplace productivity, and unemployment)—was estimated to be $62.7 billion in 2002.
The book and film A Beautiful Mind chronicle the life of John Forbes Nash, a Nobel Prize-winning mathematician who was diagnosed with schizophrenia.